6 Children’s Mental Health
Warning: This chapter contains information about childhood trauma that may be triggering for some readers.
Learning Objectives
By the end of this chapter, you should be able to:
- Discuss what mental health is and what that looks like during early childhood.
- Explain how mental health practices should begin during infancy.
- Describe mental health problems that young children may experience.
- Examine the impact of adverse childhood experiences, trauma, and stress on your children.
- Reflect on how to support young children’s resilience and social and emotional competence.
- Outline ways early care and education programs should be supporting young children’s mental health (including engaging families).
- Explain what trauma-informed care is.
 |
Licensing Regulations WAC regulations that relate to this chapter include:
110-300-0085 Family partnerships and communication.
110-300-0330 Personal relationships and child guidance.
110-300-0325 Creating a climate for healthy child development.
|
Introduction
Mental health in childhood means reaching developmental and emotional milestones and learning healthy social skills and how to cope when there are problems. Mentally healthy children have a positive quality of life and can function well at home, in early care and education programs and school, and in their communities.[1]
Mental health is an important part of overall health and well-being. Mental health includes emotional, psychological, and social well-being. It affects how people think, feel, and act. It also helps determine how people handle stress, relate to others, and make healthy choices. Mental health is important at every stage of life, from childhood and adolescence through adulthood.[2] When early educators and families know more about early childhood mental health, they are better able to support children’s learning and development.[3]
Foundation for Mental Health

Beginning at birth, children need positive relationships with the adults who care for them. When children learn to recognize and share their feelings with trusted adults, they feel good about themselves. These relationships help them develop the confidence to learn new skills. Children thrive when adults support their strengths and needs. Responsive adults help children feel safe and valued and learn how to get along well with others.
Children who can manage their feelings can learn and play with peers. They are better able to plan, monitor and control their behavior. They can also adjust to changes in schedules and routines. Children who get along with adults learn to work together and follow rules. They can also show concern for, and share, take turns and compromise with other children.[4]
Mental Health from the Beginning
Infant mental health practice applies knowledge of relationships to support and enhance healthy social and emotional development and to prevent and treat mental health disorders. The following definition of infant mental health was developed by a group of experts with the common understanding that observing young children’s interactions with parents and other significant people is key for the assessment of emotional well-being.
In addition, experts also suggest keeping in mind the infants’ underlying biology that could include temperament and compromises to resilience from early trauma. Infant mental health is the developing capacity of the child from birth to three to: experience, regulate, and express emotions; form close and secure interpersonal relationships; and explore the environment and learn—all in the context of family, community, and cultural expectations for young children. Infant mental health is synonymous with healthy social and emotional development. (ZERO TO THREE Infant Mental Health Task Force, December, 2001) The mental and physical health of infants and toddlers is critically influenced by the daily behaviors of their caregivers.
The following sections describe key concepts related to the mental health of infants. These concepts enhance what is included in the previous definition:
- “Developing capacity” highlights the extraordinarily rapid pace of growth and change in the first 3 years. Although newborns experience intense feelings and are active partners in their relationships with adults, the differentiation and complexity of a young child’s emotional and social development increases markedly over time.
- Infants and toddlers initially depend heavily on adults to help them experience, regulate, and express emotions. Infants’ cries and coos evoke strong reactions in their caregivers. An infant’s ability to master feelings develops through give and take.
- Through relationships with parents and other caregivers, infants and toddlers learn what people expect of them and what they can expect of other people. Infants and toddlers learn through what they experience within relationships and what they observe in adult’s interactions with one another.
- Infants and toddlers share and communicate feelings and experiences with significant caregivers and other children. Infants and toddlers interact with one another in emotionally meaningful ways. Parents and caregivers help young children name the feelings and understand their effect on others.
- The drive to explore and master one’s environment is inborn in humans. An essential component of infants’ and toddlers’ well-being is the self-esteem that grows out of mastering their bodies and the environment as well as sharing that mastery with parents and significant caregivers.
- Every child is a unique blend of characteristics; infants’ and toddlers’ developmental pathways will reflect not only their individual constitutional differences but also the contributions of their caregiving environments. Temperament, or the way an individual approaches the world, influences how tentatively or vigorously an infant might engage with a new person, toy, or situation.
- The state of adults’ emotional well-being and life circumstances profoundly affects the quality of infant-caregiver relationships as well as infant and toddler mental health. Parents and other significant caregivers bring their own temperament and past experiences to relationships.
- Culture influences every aspect of human development. This broad influence affects the way that infant mental health is understood; the goals and expectations adults have for young children’s development; and the childrearing practices that parents and caregivers use to promote, protect, or restore infants’ and toddlers’ mental health.[5]
 |
Reflective Practice
How does this child’s exploration relate to her self-esteem?  |
Mental Health in Early Childhood
Early childhood mental health (birth to 5 years) is a child’s growing capacity to do these things, all in the cultural context of family and community (adapted from ZERO TO THREE):
- Experience, regulate, and express emotions
- Develop close, secure, relationships
- Explore the surroundings and learn.
Early childhood mental health is the same as social emotional development.[6] Social and emotional development is important to early learning. Many social-emotional qualities—such as curiosity; self-confidence as a learner; self-control of attention, thinking, and impulses; and initiative in developing new ideas—are essential to learning at any age. Learning, problem solving, and creativity rely on these social-emotional and motivational qualities as well as basic cognitive skills.
When learning occurs in groups, such as in preschool classrooms or family child care programs, the social environment significantly influences how learning occurs. When young children enjoy interacting with adults and other children, they are more enthusiastic about activities and participate more. Furthermore, the interest and enthusiasm of others fuels the child’s own excitement about learning, and children are also motivated by others’ acknowledgment of the child’s accomplishments.[7]
It is important because it affects a child’s ability to:
- Express their needs
- Pay attention
- Solve problems
- Get along with others
- Follow directions
- Persist when challenged
- Manage their emotions
- Take initiative
- Be curious and interested in learning[8]
Interviews with preschool and kindergarten teachers indicate that children who have the greatest difficulties in learning are hindered by the lack of these social-emotional qualities more than by the inability to identify letters or numbers. Children who are delayed or impaired in developing these social-emotional and motivational qualities:
- may have difficulty controlling their emotions or behavior,
- may not readily work independently or in a group,
- often appear to lack curiosity or be uninterested in learning, and
- may have difficulties getting along with others, which may undermine the learning environment for all children[9]
Children’s mental health is critical to their later school success as well. Children who
- are able to follow directions and pay attention are able to focus on learning.
- can express their feelings are able to get help when they need it.
- learn to persist when frustrated can overcome challenges.
- feel good about themselves are able to work on their own.
- can control their behavior are able to stay on task.[10]
Finally, the importance of social-emotional development to early learning is consistent with the research on brain science. The developing brain is not neatly divided into separate areas governing learning, thinking, and emotions. Instead, it is a highly interconnected organ with different regions influencing, and being affected by, the others. This means, for example, that young children who experience emotional challenges (perhaps because of stress) are less ready for learning because brain regions related to memory are being affected by other regions governing emotion. This conclusion from brain research is, of course, consistent with the everyday experience of teachers of children whose stressful lives often lead to emotional, behavioral, and learning difficulties.[11]
Childhood Mental Health Issues
There are two types of mental health issues this chapter is going to address. The first is diagnosable mental problems. The second is the result of Adverse Childhood Experiences and childhood trauma.
Mental Health Problems
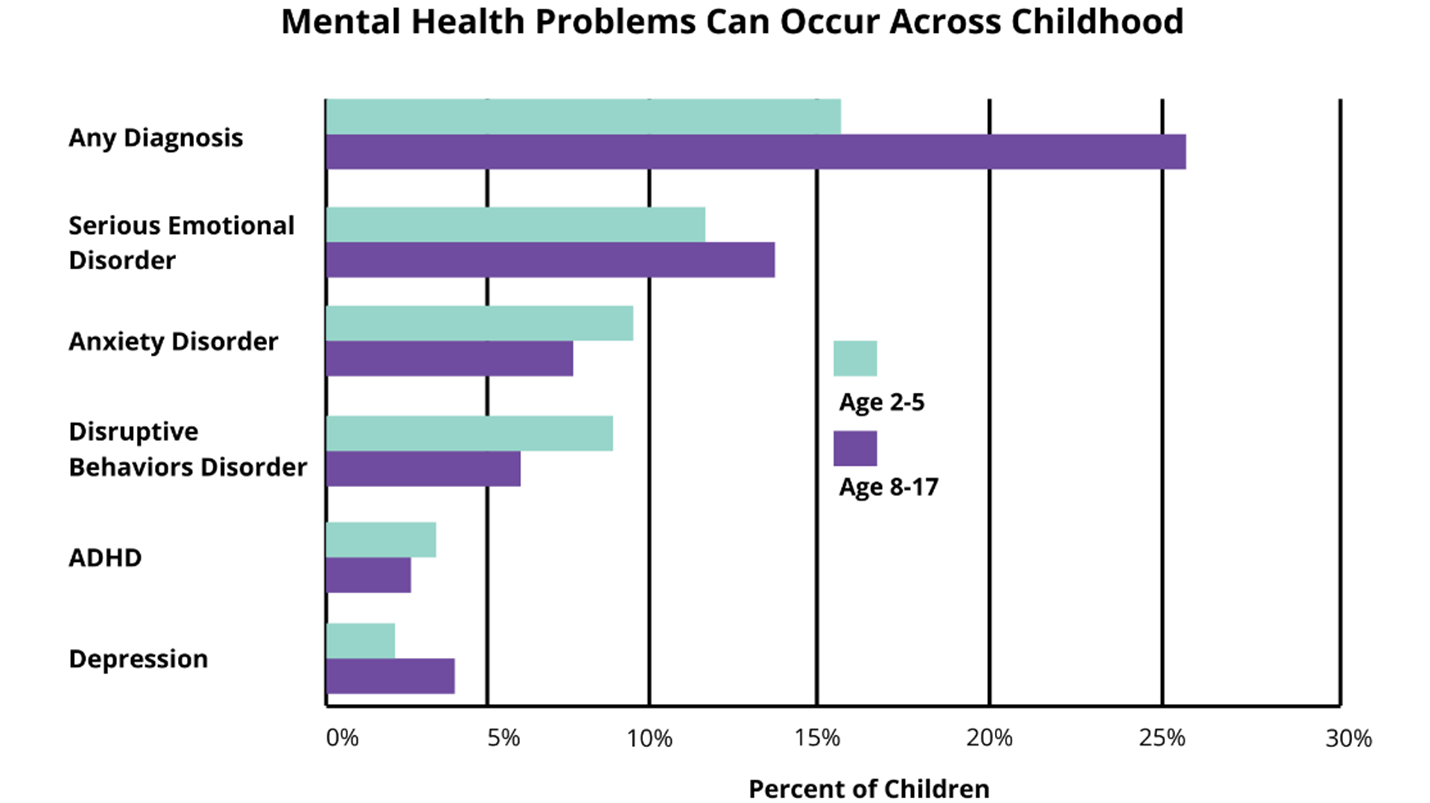
Mental health problems, which the CDC refers to as mental disorders, among children are described as serious changes in the way children typically learn, behave, or handle their emotions, which cause distress and problems getting through the day.
Among the more common mental health problems that can be diagnosed in childhood are attention-deficit/hyperactivity disorder (ADHD, which has already been addressed in Chapter 10), anxiety, and behavior disorders.[12]
Anxiety and Depression
Many children have fears and worries and may feel sad and hopeless from time to time. Strong fears may appear at different times during development. For example, toddlers are often very distressed about being away from their parents, even if they are safe and cared for. Although fears and worries are typical in children, persistent or extreme forms of fear and sadness could be due to anxiety or depression. Because the symptoms primarily involve thoughts and feelings, they are called internalizing disorders.
Anxiety
When children do not outgrow the fears and worries that are typical in young children, or when there are so many fears and worries that they interfere with school, home, or play activities, the child may be diagnosed with an anxiety disorder. Examples of different types of anxiety disorders include:
- Being very afraid when away from parents (separation anxiety)
- Having extreme fear about a specific thing or situation, such as dogs, insects, or going to the doctor (phobias)
- Being very afraid of school and other places where there are people (social anxiety)
- Being very worried about the future and about bad things happening (general anxiety)
- Having repeated episodes of sudden, unexpected, intense fear that come with symptoms like heart pounding, having trouble breathing, or feeling dizzy, shaky, or sweaty (panic disorder)
Anxiety may present as fear or worry but can also make children irritable and angry. Anxiety symptoms can also include trouble sleeping, as well as physical symptoms like fatigue, headaches, or stomachaches. Some anxious children keep their worries to themselves and, thus, the symptoms can be missed.
Depression

Occasionally being sad or feeling hopeless is a part of every child’s life. However, some children feel sad or uninterested in things that they used to enjoy or feel helpless or hopeless in situations they are able to change. When children feel persistent sadness and hopelessness, they may be diagnosed with depression.
Examples of behaviors often seen in children with depression include:
- Feeling sad, hopeless, or irritable a lot of the time
- Not wanting to do or enjoy doing fun things
- Showing changes in eating patterns – eating a lot more or a lot less than usual
- Showing changes in sleep patterns – sleeping a lot more or a lot less than normal
- Showing changes in energy – being tired and sluggish or tense and restless a lot of the time
- Having a hard time paying attention
- Feeling worthless, useless, or guilty
- Showing self-injury and self-destructive behavior
Extreme depression can lead a child to think about suicide or plan for suicide. While less common in early childhood, for youth ages 10-24 years, suicide is among the leading causes of death.
Some children may not talk about their helpless and hopeless thoughts and may not appear sad. Depression might also cause a child to make trouble or act unmotivated, causing others not to notice that the child is depressed or to incorrectly label the child as a troublemaker or lazy. 237
Behavior or Conduct Problems
Children sometimes argue, are aggressive, or act angry or defiant around adults. A behavior disorder may be diagnosed when these disruptive behaviors are uncommon for the child’s age at the time, persist over time, or are severe. Because disruptive behavior disorders involve acting out and showing unwanted behavior towards others, they are often called externalizing disorders.
Oppositional Defiant Disorder
When children act out persistently so that it causes serious problems at home, in school, or with peers, they may be diagnosed with Oppositional Defiant Disorder (ODD). ODD usually starts before 8 years of age, but no later than by about 12 years of age. Children with ODD are more likely to act oppositional or defiant around people they know well, such as family members, a regular care provider, or a teacher. Children with ODD show these behaviors more often than other children their age.
Examples of ODD behaviors include:
- Often being angry or losing one’s temper
- Often arguing with adults or refusing to comply with adults’ rules or requests
- Often resentful or spiteful
- Deliberately annoying others or becoming annoyed with others
- Often blaming other people for one’s own mistakes or misbehavior
Conduct Disorder
Conduct Disorder (CD) is diagnosed when children show an ongoing pattern of aggression toward others, and serious violations of rules and social norms at home, in school, and with peers. In older children, these rule violations may involve breaking the law and result in arrest. Children with CD are more likely to get injured and may have difficulties getting along with peers.
Examples of CD behaviors include:
- Breaking serious rules, such as running away, or for older children staying out at night when told not to or skipping school
- Being aggressive in a way that causes harm, such as bullying, fighting, or being cruel to animals
- Lying, stealing, or damaging other people’s property on purpose[13]
Obsessive-Compulsive Disorder (OCD)
Many children occasionally have thoughts that bother them, and they might feel like they have to do something about those thoughts, even if their actions don’t actually make sense. For example, they might worry about having bad luck if they don’t wear a favorite piece of clothing. For some children, the thoughts and the urges to perform certain actions persist, even if they try to ignore them or make them go away. Children may have an obsessive-compulsive disorder (OCD) when unwanted thoughts, and the behaviors they feel they must do because of the thoughts, happen frequently, take up a lot of time (more than an hour a day), interfere with their activities, or make them very upset. The thoughts are called obsessions. The behaviors are called compulsions.
Having OCD means having obsessions, compulsions, or both. Examples of obsessive or compulsive behaviors include:
- Having unwanted thoughts, impulses, or images that occur over and over and which cause anxiety or distress.
- Having to think about or say something over and over (for example, counting, or repeating words over and over silently or out loud)
- Having to do something over and over (for example, handwashing, placing things in a specific order, or checking the same things over and over, like whether a door is locked)
- Having to do something over and over according to certain rules that must be followed exactly in order to make an obsession go away.
Children do these behaviors because they have the feeling that the behaviors will prevent bad things from happening or will make them feel better. However, the behavior is not typically connected to actual danger of something bad happening, or the behavior is extreme, such as washing hands multiple times per hour.
A common myth is that OCD means being really neat and orderly. Sometimes, OCD behaviors may involve cleaning, but many times someone with OCD is too focused on one thing that must be done over and over, rather than on being organized. Obsessions and compulsions can also change over time.[14]
Post-Traumatic Stress Disorder (PTSD)
All children may experience very stressful events that affect how they think and feel. Most of the time, children recover quickly and well. However, sometimes children who experience severe stress, such as from an injury, from the death or threatened death of a close family member or friend, or from violence, will be affected long-term. The child could experience this trauma directly or could witness it happening to someone else. When children develop long term symptoms (longer than one month) from such stress, which are upsetting or interfere with their relationships and activities, they may be diagnosed with post-traumatic stress disorder (PTSD).

Examples of PTSD symptoms include:
- Reliving the event over and over in thought or in play
- Nightmares and sleep problems
- Becoming very upset when something causes memories of the event
- Lack of positive emotions
- Intense ongoing fear or sadness
- Irritability and angry outbursts
- Constantly looking for possible threats, being easily startled
- Acting helpless, hopeless or withdrawn
- Denying that the event happened or feeling numb
- Avoiding places or people associated with the event
Because children who have experienced traumatic stress may seem restless, fidgety, or have trouble paying attention and staying organized, the symptoms of traumatic stress can be confused with symptoms of attention-deficit/hyperactivity disorder (ADHD).
Examples of events that could cause PTSD include:
- Physical, sexual, or emotional maltreatment
- Being a victim or witness to violence or crime
- Serious illness or death of a close family member or friend
- Natural or manmade disasters
- Severe car accidents[15]
Diagnosis and Treatment of Mental Health Problems in Childhood
Symptoms of mental health problems change over time as a child grows, and may include difficulties with how a child plays, learns, speaks, and acts or how the child handles their emotions. Symptoms often start in early childhood, although some disorders may develop during the teenage years. The diagnosis is often made in the school years and sometimes earlier. However, some children with a mental disorder may not be recognized or diagnosed as having one.
Childhood mental health problems can, and should, be treated and managed. There are many treatment options based on the best and most current medical evidence, so families and doctors should work closely with everyone involved in the child’s treatment — teachers, coaches, therapists, and other service providers. Taking advantage of all the resources available will help parents, health professionals, and educators guide the child towards success. Early diagnosis and appropriate services for children and their families can make a difference in the lives of children with mental disorders and their families.[16]
Adverse Childhood Experiences and Trauma
The childhood years, from the prenatal period to late adolescence, are the “building block” years that help set the stage for adult relationships, behaviors, health, and social outcomes.[17] The occurrence of Adverse Childhood Experiences and childhood trauma can damage those building blocks. Early care and education programs can help children develop resilience to combat the negative effects of those.
Adverse Childhood Experiences
Adverse Childhood Experiences, or ACEs, are potentially traumatic events that occur in childhood (0-17 years) such as experiencing violence, abuse, or neglect; witnessing violence in the home; and having a family member attempt or die by suicide. Also included are aspects of the child’s environment that can undermine their sense of safety, stability, and bonding such as growing up in a household with substance misuse, mental health problems, or instability due to parental separation or incarceration of a parent, sibling or other member of the household.
Traumatic events in childhood can be emotionally painful or distressing and can have effects that persist for years. Factors such as the nature, frequency and seriousness of the traumatic event, prior history of trauma, and available family and community supports can shape a child’s response to trauma.[18]
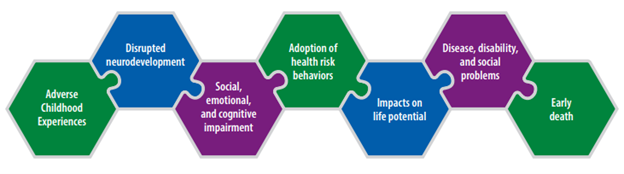
Adverse Childhood Experiences and associated conditions such as living in under-resourced or racially segregated neighborhoods, frequently moving, experiencing food insecurity, and other instability can cause toxic stress (i.e., prolonged activation of the stress-response system). Some children may face further exposure to toxic stress from historical and ongoing traumas due to systemic racism or the impacts of multigenerational poverty resulting from limited educational and economic opportunities.
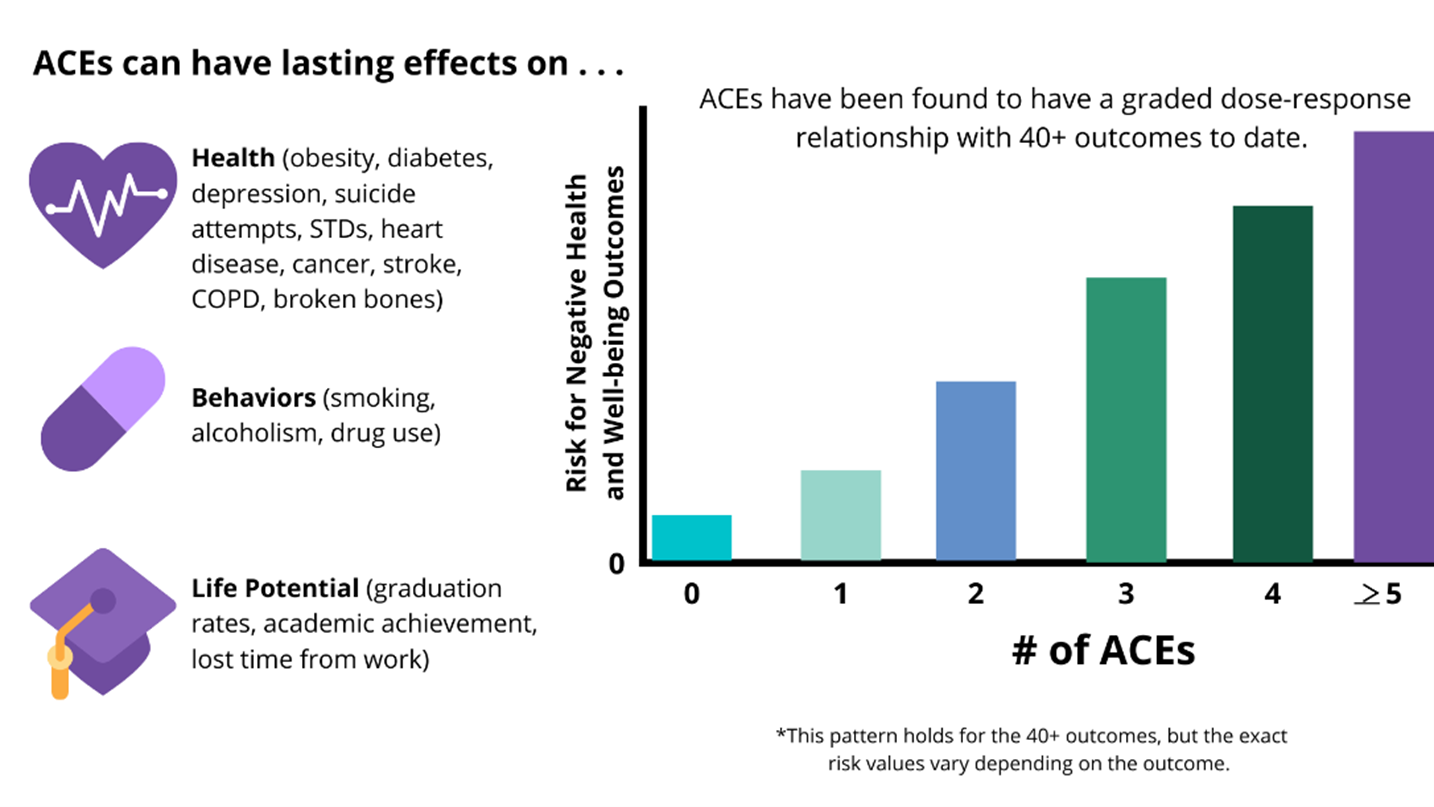
A large and growing body of research indicates that toxic stress during childhood can harm the most basic levels of the nervous, endocrine, and immune systems, and that such exposures can even alter the physical structure of DNA (epigenetic effects). Changes to the brain from toxic stress can affect such things as attention, impulsive behavior, decision-making, learning, emotion, and response to stress. Absent factors that can prevent or reduce toxic stress, children growing up under these conditions often struggle to learn and complete schooling. They are at increased risk of becoming involved in crime and violence, using alcohol or drugs, and engaging in other health-risk behaviors (e.g., early initiation of sexual activity; unprotected sex; and suicide attempts). They are susceptible to disease, illness, and mental health challenges over their lifetime. Children growing up with toxic stress may have difficulty forming healthy and stable relationships. They may also have unstable work histories as adults and struggle with finances, family, jobs, and depression throughout life—the effects of which can be passed on to their own children.[19]
 |
Reflective Practice If it feels safe to you, find your own ACE score using the assessment at Finding-Your-Ace-Score.pdf (ncjfcj.org). What impact do you think this had and/or still has on you? What might this mean for you when you care for young children who have their own ACEs and trauma? |
Childhood Trauma
Childhood trauma occurs when a child experiences an actual or threatened negative event, series of events, or set of circumstances that cause emotional pain and overwhelm the child’s ability to cope. Childhood trauma is widespread and can take many forms. Common types of childhood trauma include:
- Abuse and neglect
- Family violence
- Community violence
- School violence
- Life-threatening accidents and injuries
- Frightening or painful medical procedures
- Serious and untreated parental mental illness
- Loss of or separation from a parent or other loved one
- Natural or manmade disasters
- War or terrorist attack
- Forced displacement or refugee status
- Discrimination
- Extreme poverty
Trauma exposure often begins early in life. Young children are at the highest risk for exposure to trauma and are most vulnerable to its adverse effects. An estimated half of all children in the United States—approximately 35 million—are exposed to at least one type of trauma prior to their eighth birthday. For example, child abuse and neglect are most common among children younger than age 3. Children under age 5 are most likely to incur injuries from falls, choking, and poisoning, and represent the majority of children who witness domestic violence. Children from certain racial and ethnic groups also are more likely to experience adversities that can cause trauma. For example, exposure to childhood adversity is more common among black and Hispanic children than among white children, even when accounting for the role of income.
Childhood trauma is strongly linked to mental and physical health problems over the lifespan. It negatively impacts brain development, cognitive development, learning, social-emotional development, the ability to develop secure attachments to others, and physical health; it is also associated with a shortened lifespan. A considerable body of research demonstrates that children suffer the most severe, long-lasting, and harmful effects when trauma exposure begins early in life, takes multiple forms, is severe and pervasive, and involves harm by a parent or other primary caregiver—often referred to as complex trauma.
Childhood trauma is more likely to lead to post-traumatic stress disorder (PTSD) than trauma that occurs in adulthood. Children exposed to several different forms of trauma are more likely to exhibit PTSD (e.g., anxiety, depression, anger, aggression, dissociation) than children with chronic exposure to a single type of trauma. Children and youth with PTSD may re-experience the traumatic event through intrusive memories, nightmares, and flashbacks; avoid situations or people that remind them of the trauma; and feel intense anxiety that disrupts their everyday lives. In addition, they may engage in aggressive, self-destructive, or reckless behavior; have trouble sleeping; or remain in a state of hypervigilance, an exaggerated state of awareness and reactivity to their environments. However, there is no typical reaction to trauma. The vast majority of children show distress immediately following a traumatic event, but most return to their prior level of functioning.
Generally, children’s reactions to trauma differ based on the nature of the trauma; the child’s individual, family, and neighborhood characteristics; and the overall balance of risk and protective factors in their lives. It also depends on their age and developmental stage.
Young children who experience trauma may:
- Have difficulties forming an attachment to caregivers
- Experience excessive fear of strangers or separation anxiety
- Have trouble eating and sleeping
- Be especially fussy
- Show regression after reaching a developmental milestone (e.g., sleeping through the night, toilet training)
- School-age children who experience trauma may:
- Engage in aggressive behavior
- Become withdrawn
- Fixate on their own safety or the safety of others
- Re-enact the traumatic event through play
- Have frequent nightmares
- Exhibit difficulty concentrating in school
Table 6.1 – Childhood trauma has many effects[20]
| Domain | Impact |
| Brain Development |
|
| Cognition |
|
| Physical Health |
|
| Emotions |
|
| Relationships |
|
| Mental Health |
|
| Behavior |
|
Resilience to Childhood Trauma
When parents, service providers, and programs employ a resilience framework to childhood trauma, they understand there are always opportunities to support positive developmental trajectories among children, even if they have experienced trauma. Resilience has been defined as “adynamic process encompassing positive adaptation within the context of significant adversity.” Resilience is not a personal trait that individuals do or do not possess (thus, the term “resiliency” is best avoided because it connotes an individual characteristic), but rather a product of interacting factors—biological, psychological, social, and cultural—that determine how a child responds to traumatic events.
Resilience to trauma can be defined in several ways: positive child outcomes despite exposure to trauma, prevention of trauma recurrence despite high risk for further exposure, or avoidance of traumatic experiences altogether in the face of significant risk. All three of these conceptualizations of resilience are based on an ecological approach.
Using an ecological approach to promote resilience in development among children who experience trauma is useful because it assumes that there are multiple levels of influence on a child’s development—the individual, parent, family, school, community, and culture—which may increase or decrease a child’s risk for and response to experiencing trauma. These various influences are often referred to as risk and protective factors.
Risk factors are circumstances, characteristics, conditions, events, or traits at the individual, family, community, or cultural level that may increase the likelihood a person will experience adversity (e.g., childhood trauma, re-traumatization, or negative outcomes due to trauma). Risk factors for specific types of trauma may vary, but commonly include living in poverty, a lack of social supports, and prior history of trauma. Additionally, children who identify as lesbian, gay, bisexual, transgender, or queer (LGBTQ) and children in military families are at an increased risk for experiencing trauma. However, the presence of risk factors or membership in a high-risk group does not necessarily mean that a child will experience trauma or its most adverse effects. Protective factors can buffer children from risk and improve the odds of resilient functioning.
Protective factors are characteristics, conditions, or events that promote healthy development and minimize the risk or likelihood a person will experience a particular illness or event, or its related negative outcomes. Research shows that the strongest protective factor linked with resilience to childhood trauma is the reliable presence of a sensitive, nurturing, and responsive adult. The presence of such a figure can help children by restoring a sense of safety, predictability, and control; giving them the feeling of safety; providing them a way to process traumatic events; protecting them from re-traumatization; supporting their development of self-regulation; and helping them heal.
In addition, the National Child Traumatic Stress Network highlights the following protective factors that promote resilience to childhood trauma:
- Support from family, friends, people at school, and members of the community
- A sense of safety at home, at school, and in the community
- High self-esteem and positive sense of self-worth
- Self-efficacy
- Spiritual or cultural beliefs, goals, or dreams for the future that provide a sense of meaning to a child’s life
- A talent or skill in a particular area (e.g., excelling in school or in a sport)
- Coping skills that can be applied to varying situations
Finally, resilience to childhood trauma depends largely on the supports available to a child and his or her family. Family members, teachers, mental health providers, child welfare workers, and other community service providers can work together to ensure that children and families receive the emotional and concrete supports (e.g., food, shelter, financial stability) they need. This system of care approach is also a cornerstone of TIC.[21]
 |
Reflective Practice
What risk factors did you encounter in your own childhood? What protective factors did you experience? How did/does this effect your resilience? |
Early Care and Education’s Role in Children’s Mental Health
Many practices of high-quality early care and education programs promote mental health and well-being including:
- Screening and assessment of infants’ and toddlers’ social and emotional well-being support the functions of promotion, prevention, and intervention.
- integrating curriculum and individualization.
- A well-designed space is comfortable for infants and toddlers with different temperaments as well as for their teachers and parents.
- Poorly designed environments are stressful. Teachers are concerned about the safety and well-being of children, and their saying “no” occupies a great deal of teacher energy and attention. The time teachers spend monitoring keeps them from interacting with an infant or toddler in ways that build self-esteem.
- Having partnerships with community resources that families can be referred to.
- Reciprocal communication with families.[22]
Mental health services in early care and education programs can address:
- Promotion—helping all children to feel good about themselves, to get along with others and to manage their behavior.
- Prevention—reducing the likelihood that children will develop mental health problems and reducing the impact of mental health problems that do exist.
- Early Identification—paying attention to mental health problems early on.
- Treatment—helping connect families with appropriate help for children with mental health problems.[23]
Table 6.2 – Nine Things Early Care and Education Programs Should Know[24]
| Nine Things Early Care and Education Programs Should Know |
| Mental health is an essential part of health. |
| The mental health of young children is linked to the wellbeing of the people who care for them. |
| Promoting the mental health of infants and young children can make a positive difference for years to come. |
| Positive relationships support positive mental health. |
| Culture plays an important role in young children’s mental health and in how families view mental health and behavior. |
| The more staff and families know about mental health the better they are able to support it. |
| Addressing mental health concerns when children are young is more effective than waiting until they are older. |
| Mental health must be an integral part of early care and education programs. |
| Programs that focus on mental health are able to design services that improve children’s behavior. |
 |
Infant and Early Childhood Mental Health Consultation
Infant and Early Childhood Mental Health Consultation (IECMHC) a prevention-based service that pairs a mental health consultant with families and adults who work with infants and young children in the different settings where they learn and grow, such as child care, preschool, and their home. The aim is to build adults’ capacity to strengthen and support the healthy social and emotional development of children―early and before intervention is needed.
IECMHC has been shown to improve children’s social skills and emotional functioning, promote healthy relationships, reduce challenging behaviors, reduce the number of suspensions and expulsions, improve classroom quality, and reduce provider stress, burnout, and turnover.[25] |
Increasing Children’s Opportunities to Practice Social Skills and Emotional Competencies
Everyday activities in the classroom can be planned and implemented to help children’s social and emotional development (which, as mentioned, is the same as their mental health).
Teaching Children About Emotions
There are many things that teachers can do to help support children’s understanding emotions. Here are some ideas:
- Make faces expressing different emotions and have children guess what you might be feeling.
- Throughout the day, help children learn to label their own emotions (e.g., “It looks like you are feeling mad that we can’t go outside; what can we do to help you feel better?”).
- While reading stories to children, have children guess how the characters in the story are feeling. Ask questions like, “How can you tell that the character is feeling that way? Can you make a face that shows that feeling?”
- Use puppets to act out different situations; for example, one puppet takes a toy from another puppet. Ask the children what emotion(s) the puppets might be feeling.
- Frequently direct children to look at each other’s faces and think about how they are feeling.
- Listen to some different types of music, such as rock or classical, and let the children dance to the music. Ask children how the song made the children feel.
Teaching Children about Friendship
Being in an environment with many same-aged peers that are all learning about how to express themselves, work with others, and regulate their behaviors provides a great place to help children learn about friendships. Here are some ideas:
- Model asking others for help. If you have a task to do in the classroom, involve another child.

Figure 6.8 When children work together, they practice their social skills. - Whenever children have to take turns, have the child who just finished call someone to go next.
- Have children help during routines such as putting out cots or mats for naptime.
- Talk about your own social behaviors. You can say things like, “I said ‘thank you’ to Ms. Tanya because she passed me the milk,” or “I think I’ll hold the door open for Jamal because his hands are full.”
- Identify certain items in centers that require children to help each other, like taking a dollhouse off a shelf, moving the car garage, or feeding the class pet. Explain to children that it takes two friends to do these things.
- Provide toys and play games that require two or more people, like a wagon or toss and catch game.
- Make a “Friendship Board” on a bulletin board in your classroom. Take pictures when children are working together on something or playing together and put them on the wall.
Teaching Children about Problem-Solving
Everyday life presents many opportunities for children to engage in identifying problems and generating and trying out solutions. Here are some ideas for in the classroom:
-

Figure 6.9 Use real life opportunities to help children practice problem-solving. Use naturally occurring opportunities to work problem-solving words into the classroom vocabulary. When there aren’t enough glue sticks or too many people wanting to go in a certain center, say things like, “We have a problem. What can we do to fix it?”
- Use naturally occurring problems in small groups to brainstorm possible solutions. Talk about that problem and come up with some ideas that could work to solve the problem.
- Use puppets to act out problem situations during group time. Ask the children to come up with a solution for the problem.
- When a child asks for help, take the opportunity to involve another child in solving the problem. You can say, “Let’s look and see if one of your friends can help you. Marne, Sheila needs a glue stick and there are no more. Can you help her solve her problem?”
- Encourage the children while they are working through a problem and provide them with recognition when they solve it. You can use a situation that ended well as an example to discuss in large group.
- Discuss the problems that characters are having in the books you are reading. Brainstorm some possible solutions and guess what they are going to do.
- Make up a song about what to do when children have a problem. For example, to the Row, Row, Row Your Boat tune: “Problem, problem, problem, oh what can we do? Stop and think of something new. I’ll try it out with you.”
- If similar solutions keep coming up during discussions of problem-solving, start a “Solution Board” that shows the different solutions with an image to represent it. Children can use it to help think of solutions as problems arise, and the teacher can prompt a child to go look at it.
Teaching Children about Handling Disappointment and Difficult Emotions
Handling intense emotions and the disappointment when things don’t go their way are challenging for young children (and even adults!) to navigate. But teachers can help children develop techniques to handle difficult emotions. Here are some ideas:
- Throughout the day, model labeling your own emotions. For example, “I feel frustrated because I cannot open this jar of paint.”
- Help children learn to label their emotions when they have conflict with other children: “Bobby, it looks like you are feeling angry because Terrence took away your toy. Can you tell Terrence how it makes you feel when he takes your toy away?”
- When children cry, identify their feelings, and yours too. “I know that was really scary falling off the slide. I was worried about you. I am glad you are okay. Is there something I can do to help you until you feel better?”
- Help children learn how to take deep breaths by “smelling the flowers” and “blowing out the birthday candles.” Knowing how to breathe deeply is an important part of learning how to calm down when angry or upset.
- Give children materials to use to get out their anger. They can use a toy hammer, squeeze playdough, or run laps at recess. Let them know that it is okay to be angry and that there are safe ways to express anger.
- Act out the difference between feeling tense (like a robot or statue) and relaxed (like a rag doll or stuffed animal). Have children act it out, too, so they begin to learn to identify when they are becoming wound up.
- Help children learn to label their own emotions. You can say, “It looks like you are really frustrated over here. What is the problem?”
- Give children different situations, such as “A child is very sad because he misses his mom,” and let them act it out. Talk about the emotion and some things the child might do to feel better.
- Children’s storybooks have lots of opportunities to talk about dealing with certain emotions. Point out characters’ simple emotions like happy, sad, mad, and excited, and look for opportunities to label more complex ones like disappointed, frustrated, surprised, and embarrassed. See what the characters do to deal with those emotions and whether or not the children think it was a good way. Brainstorm other things that could have been done when the characters were feeling that way.
- If children are feeling sad at drop-off, have them “write” a letter or draw a picture to show their caregivers at pick-up time. Talk about how it is ok to feel sad, but that their caregiver will come back at the end of the day.[26]
 |
Engaging Families in Supporting Children’s Social Emotional Development
There are many things you can do to give families ideas of how to support their children’s social and emotional development at home too. You can
Some specific ideas you can give parents include the following:
|
Supporting Children Under Stress
Supporting children’s mental health also extends to helping children deal with the stress that they may encounter. One of the most important things teachers can do is provide the child with a predictable, safe haven where children can feel secure. Teachers can create a comfortable and comforting everyday routine that is child-centered, individualized, responsive, and helpfully structured to give young children a sense of control and predictability that may be lacking in other aspects of the child’s life. Central to these efforts is providing children with supportive adult relationships that are reliable and helpful. This may be more difficult than one would expect because young children under stress often test these relationships to see whether teachers and other adults will remain responsive to them even when children act defiantly or negatively.
In some circumstances, it can be helpful for teachers to obtain the advice of an early childhood mental health consultant who can observe the child in the classroom, talk with the teacher about the child’s behavior, and suggest strategies for providing supportive assistance. Early childhood mental health consultants can be valuable resources to an early childhood education program. They can help teachers provide much-needed support to young children who may not have other such sources of support elsewhere in their lives.[28]
Trauma-Informed Care
As mentioned, children who are exposed to traumatic life events are at significant risk for developing serious and long-lasting problems across multiple areas of development. However, children are far more likely to exhibit resilience to childhood trauma when child-serving programs, institutions, and service systems understand the impact of childhood trauma, share common ways to talk and think about trauma, and thoroughly integrate effective practices and policies to address it—an approach often referred to as trauma-informed care (TIC).
The context in which children live, learn, and grow shapes both their immediate and long-term well-being. Accordingly, children who experience trauma are more likely to exhibit resilience when their environments are responsive to their specific needs. Families, schools, community-based programs and services, and the individuals caring for children can increase the chances of resilience following childhood trauma when they become aware of the impact of childhood trauma, provide a sense of safety and predictability, protect children from further adversity, and offer pathways for their recovery. In other words, children benefit when these entities provide them with trauma-informed care (TIC).
Despite its focus on trauma, TIC is inherently a strengths-based perspective that emphasizes resilience instead of pathology. TIC has been defined and implemented in a number of ways, but the Substance Abuse and Mental Health Services Administration has identified four key elements—the Four Rs (see Figure 6.9)
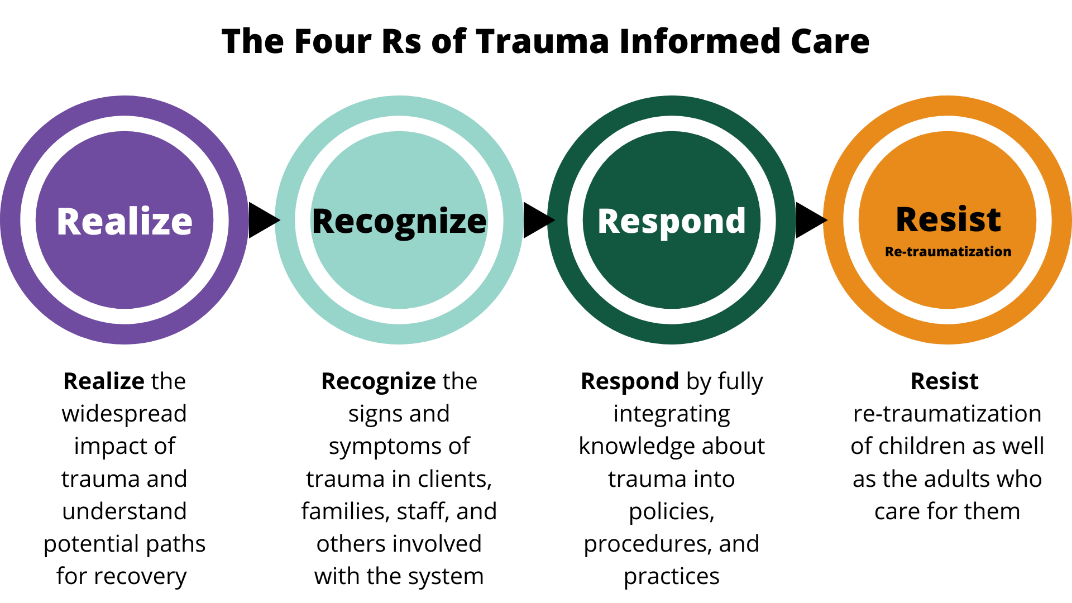
Applying TIC to real-world settings begins with a child’s first contact with a program, institution, or service system. It requires a comprehensive and multi-pronged effort involving the many adults in children’s lives. For example, in a school or afterschool program, TIC means increasing trauma-related knowledge and skills among program facilitators, school administrators, bus drivers, food service workers, classroom assistants, administrative staff, volunteers, teachers, leadership, special education professionals, school social workers and psychologists, families, and anyone else who comes into contact with children. However, increasing trauma knowledge is only one aspect of TIC, which also means that the individuals who care for children must be able to:
- Realize the widespread nature of childhood trauma and how it impacts the child’s emotional, social, behavioral, cognitive, brain, and physical development, as well as their mental health. In addition, adults must be aware of the influence of trauma on family members, first responders, service providers, and others who may experience secondary stress (trauma-related reactions to exposure to another person’s traumatic experience). In some instances, adults endure the same traumatic events or circumstances as the child (e.g., a natural disaster, community violence, death of a community member) and may benefit from similar supports.
- Recognize the symptoms of trauma, including how trauma reactions (i.e., symptoms of posttraumatic stress) vary by gender, age, type of trauma, or setting. In addition, the adults in children’s lives must understand that a child’s challenging behaviors are normal, self-protective, and adaptive reactions to highly stressful situations, rather than viewing that child as intentionally misbehaving. Children’s trauma reactions are understood to be adaptive efforts to protect themselves in response to traumatic events. For example, a child may be hypervigilant to an adult’s anger or disapproval because, in the past, he or she experienced physical abuse by a parent. Or, a child may disassociate or daydream as a learned response that enables them to avoid feeling or thinking about a traumatic experience. In addition, TIC means recognizing that trauma may influence a child’s engagement in activities and services, interactions with peers and adults, and responsiveness to rules and guidelines.
- Respond by making necessary adjustments, in their own language and behavior, to the child’s environment; and to policies, procedures, and practices to support the child’s recovery and resilience to trauma.
- Resist re-traumatization by actively shaping children’s environments to avoid triggers (sounds, sights, smells, objects, places, or people that remind an individual of the original trauma) and protect children from further trauma, which can exacerbate the negative impacts of trauma and interfere with the healing process.
Training and Professional Development on Child Trauma
Providing adults (staff, leadership, families, and community partners) with training and professional development on childhood trauma is an important component of implementing TIC.[29] It is essential that adults become aware of the prevalence and impact of trauma, and learn to apply a “trauma lens” (i.e., gain the capacity to view children’s difficulties in behavior, learning, and relationships as natural reactions to trauma that warrant understanding and sensitive care). In addition, adults can learn key strategies to manage trauma-related problems in childhood. These include:
- creating environments that feel physically and emotionally safe.
- teaching children self-regulation, language and communication skills, and how to build healthy relationships.
- learning each child’s trauma triggers and how both the child and adults can limit, anticipate, and cope with them.
- supporting the development of healthy attachments with parents and other caregivers, as well as positive relationships with peers.
Evaluations of TIC initiatives also indicate that when parents, service providers, and programs share a common language and view of trauma, they are better able to work together to meet children’s needs.
Training and professional development opportunities are also important for increasing the capacity of adults to attend to other aspects of TIC, including:
- family engagement.
- practices that are responsive to culture, gender, and sexual orientation.
- collaboration with community service providers (e.g., mental health providers who can screen for childhood trauma and provide evidence-based treatment).
- developing and integrating emergency and crisis response protocols.
- establishing trauma-informed policies that support positive youth development despite exposure to trauma.
Building capacity and maintaining an ongoing commitment to TIC efforts are critical to sustainability. However, although it is a critical component of TIC, training staff and parents on the impact of childhood trauma is not sufficient and does not in and of itself constitute TIC. TIC must also include comprehensive, ongoing professional development and education for parents, families, school staff, out-of-school program staff, and community service providers on jointly addressing childhood trauma.
Secondary Traumatic Stress
TIC also means attending to the psychological and physical safety and well-being of the adults who care for children who have experienced trauma. Professionals, parents, and other caregiving adults may suffer secondary traumatic stress (trauma-related reactions to exposure to another person’s traumatic experience). The National Child Traumatic Stress Network recommends the following strategies to combat secondary traumatic stress and reduce related staff burnout and turnover:
- Provide high-quality, reflective supervision
- Maintain trauma workload balance
- Support workplace self-care groups
- Enhance the physical safety of staff
- Provide training to both staff and leadership to increase awareness about secondary traumatic stress and how to address it effectively
- Develop opportunities for staff and leadership to learn about and engage in self-care practices.
- Create external partnerships with secondary traumatic stress experts.
- Regularly assess the vulnerability and resilience of staff and leadership to second traumatic stress
- Create a buddy system for self-care accountability.[30]
 |
Reflective Practice What are some key take-aways for you about how teachers can support children’s mental health? What are some ways that you can stay mentally healthy as well? |
Summary
Children’s mental health (their social and emotional development) must be intentionally supported from the beginning. Children with mental health problems (both diagnosed and that may go undiagnosed) and children who experience adverse childhood experiences, trauma, and stress may need additional mental health support. Early care and education programs should practice trauma informed care and recognize their role in helping children, and their families, to develop resilience.
 |
Resources for Further Exploration |
- What Are Childhood Mental Disorders? by the Centers for Disease Control and Prevention is in the public domain ↵
- Mental Health by the Centers for Disease Control and Prevention is in the public domain ↵
- Promoting Children’s Social and Emotional Well-Being by Head Start Early Childhood Learning & Knowledge Center is in the public domain ↵
- Healthy Children Are Ready to Learn by the National Center on Early Childhood Health and Wellness is in the public domain ↵
- Pathways to Prevention: A Comprehensive Guide for Supporting Infant and Toddler Mental Health by ZERO TO THREE is in the public domain ↵
- Mental Health: Tips for Health Managers by the Head Start National Center on Health is in the public domain ↵
- California Preschool Curriculum Framework (Volume 1) by the California Department of Education is used with permission ↵
- Mental Health: Tips for Health Managers by the Head Start National Center on Health is in the public domain ↵
- California Preschool Curriculum Framework (Volume 1) by the California Department of Education is used with permission ↵
- Mental Health: Tips for Health Managers by the Head Start National Center on Health is in the public domain ↵
- California Preschool Curriculum Framework (Volume 1) by the California Department of Education is used with permission ↵
- What Are Childhood Mental Disorders? by the Centers for Disease Control and Prevention is in the public domain ↵
- Behavior or Conduct Problems in Children by the Centers for Disease Control and Prevention is in the public domain ↵
- Obsessive-Compulsive Disorder in Children by the Centers for Disease Control and Prevention is in the public domain ↵
- Post-Traumatic Stress Disorder in Children by the Centers for Disease Control and Prevention is in the public domain ↵
- What Are Childhood Mental Disorders? by the Centers for Disease Control and Prevention is in the public domain ↵
- Preventing Adverse Childhood Experiences (ACEs) by the CDC National Center for Injury Prevention & Control, Division of Violence Prevention, is in the public domain ↵
- Preventing Adverse Childhood Experiences (ACEs) by the CDC National Center for Injury Prevention & Control, Division of Violence Prevention, is in the public domain ↵
- Preventing Adverse Childhood Experiences (ACEs) by the CDC National Center for Injury Prevention & Control, Division of Violence Prevention, is in the public domain ↵
- “How to Implement Trauma-Informed Care to Build Resilience to Childhood Trauma,” by J. D. Bartlett and K. Steber, May 9, 2019, Child Trends, https://www.childtrends.org/publications/how-to-implement-trauma-informed-care-to-build-resilience-to-childhood-trauma. Copyright 2020 by ChildTrends. Reprinted with permission. ↵
- From “How to Implement Trauma-Informed Care to Build Resilience to Childhood Trauma,” by J. D. Bartlett and K. Steber, May 9, 2019, Child Trends, https://www.childtrends.org/publications/how-to-implement-trauma-informed-care-to-build-resilience-to-childhood-trauma. Copyright 2020 by ChildTrends. Reprinted with permission. ↵
- Mental Health: Tips for Health Managers by the Head Start National Center on Health is in the public domain ↵
- Mental Health: Tips for Health Managers by the Head Start National Center on Health is in the public domain ↵
- Mental Health: Tips for Health Managers by the Head Start National Center on Health is in the public domain ↵
- About Infant and Early Childhood Mental Health Consultation (IECMHC) by Substance Abuse and Mental Health Services Administration is in the public domain ↵
- Everyday Ideas for Increasing Children's Opportunities to Practice Social Skills and Emotional Competencies by Head Start Early Childhood Learning & Knowledge Center is in the public domain ↵
- Everyday Ideas for Increasing Children's Opportunities to Practice Social Skills and Emotional Competencies by Head Start Early Childhood Learning & Knowledge Center is in the public domain ↵
- California Preschool Curriculum Framework (Volume 1) by the California Department of Education is used with permission ↵
- https://www.childtrends.org/publications/how-to-implement-trauma-informed-care-to-build-resilience-to-childhood-trauma ↵
- From “How to Implement Trauma-Informed Care to Build Resilience to Childhood Trauma,” by J. D. Bartlett and K. Steber, May 9, 2019, Child Trends, https://www.childtrends.org/publications/how-to-implement-trauma-informed-care-to-build-resilience-to-childhood-trauma. Copyright 2020 by ChildTrends. Reprinted with permission. ↵

