13 Protecting Good Nutrition and Physical Wellness
Learning Objectives
By the end of this chapter, you should be able to:
- Explain the 5-2-1-0 recommendation.
- Discuss physical activity recommendations for young children.
- Examine both undernutrition and overnutrition as forms of malnutrition.
- Describe ways early care and education programs can educate children about nutrition.
- Distinguish food allergies from food intolerances.
- Identify strategies early care and education programs can follow to plan for caring for children food allergies, food intolerances, and iron deficiency anemia
 |
LICENSING REGULATIONS WAC regulations that relate to this chapter include:
110-300-0145 OUTDOOR EARLY LEARNING PROGRAM SPACE
110-300-0186 FOOD ALLERGIES AND SPECIAL DIETARY NEEDS
110-300-0190 PARENT OR GUARDIAN PROVIDED FOOD AND WRITTEN FOOD PLAN
|
|---|
Introduction
Healthy active living includes eating healthy foods, staying physically active, and getting enough rest. Developing healthy habits starts in early childhood. Eating well and being physically active helps a child continue to grow and learn.[1]
Healthy Active Living
Research tells us that the way young children eat, move, and sleep can impact their weight now and in the future. Early childhood is an ideal time to start healthy habits before unhealthy patterns are set.[2]
Many children in the United States do not follow the recommendations of the Dietary Guidelines for Americans. According to the CDC, on average, children consume too much fat, saturated fat, and sodium and not enough fruits, vegetables, or calcium. Children obtain 33%-35% of their calories from fat and 12%-13% from saturated fat (above the recommended levels of 30% and 10%, respectively). Only 16% of children ages 6-11 years meet the recommendation for total fat intake; only 9% of children meet the recommendation for saturated fat intake.[3]
Young children depend on parents, caregivers, and others to provide environments that foster and shape healthy habits. Early care and education programs have a responsibility to promote growth and development, make healthy foods available, and provide safe spaces for active play. Staff can help children and families by encouraging and modeling healthy eating and physical activity at the center and by providing suggestions for small, healthy steps at home.[4]
5-2-1-0 Message
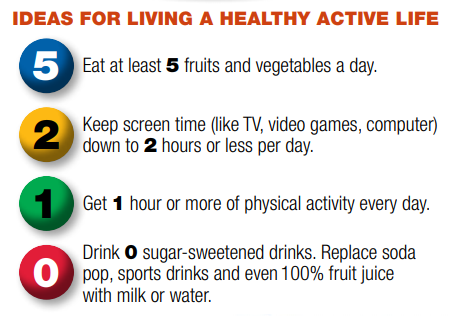
The American Academy of Pediatrics (AAP) recommends that pediatricians counsel parents and patients at every well-child check on diet and lifestyle goals as a part of obesity prevention initiatives (Hassink, 2010). These recommendations, initially put forth by the Maine Youth Overweight Collaborative obesity prevention program “Let’s Go! 5-2-1-0”, have been promoted locally and nationally for broad consumption (Rogers and Motyka, 2009).[5]
 |
ENGAGING FAMILIES IN 5-2-1-0 RECCOMMENDATIONS Share the recommendations with families with these tips.
5 Fruits and Vegetables a Day
2 Hours or Less of Screen Time a Day
1 Hour of Active Play or Physical Activity a Day
0 Sugary Drinks a Day
|
|---|
Physical Activity
Good activity habits begin early in children’s lives. As early as infancy, adults can help children grow lifelong healthy play habits. Children learn from adults, they should model being active and participate with children when possible.
Infants should spend a lot of time on the floor (and out of equipment that limits mobility). This time allows them to reach, and kick so they can reach important milestones like crawling and sitting up.
Even very active toddlers need environments that support movement and activity and intentional opportunities to be physically active. Things like dancing, jumping, and taking walks are great ways to keep them moving.[7]
Childhood and adolescence are critical periods for developing movement skills, learning healthy habits, and establishing a firm foundation for lifelong health and well-being. Regular physical activity in children and adolescents promotes health and fitness. Compared to those who are inactive, physically active youth have higher levels of cardiorespiratory fitness and stronger muscles. They also typically have lower body fat and stronger bones. Physical activity also has brain health benefits for school-aged children, including improved cognition and reduced symptoms of depression. Evidence indicates that both acute bouts and regular moderate-to-vigorous physical activity improve the cognitive functions of memory, executive function, processing speed, attention, and academic performance for these children.
Youth who are regularly active also have a better chance of a healthy adulthood. Children and adolescents do not usually develop chronic diseases, such as heart disease, hypertension, type 2 diabetes, or osteoporosis. However, current evidence shows that obesity and other risk factors for these diseases, such as elevated insulin, blood lipids, and blood pressure, are increasingly appearing in children and adolescents. Exercise training in youth with overweight or obesity can improve body composition by reducing overall levels of body fat as well as abdominal fat. Regular physical activity also makes it less likely that these risk factors will develop and more likely that children remain healthy when they become adults.

Preschool-aged children (ages 3 through 5 years) should be encouraged to move and engage in active play as well as in structured activities, such as throwing games and bicycle or tricycle riding. To strengthen bones, young children should do activities that involve hopping, skipping, jumping, and tumbling. Although the specific amount of activity needed to improve bone health and avoid excess fat in young children is not well defined, a reasonable target may be 3 hours per day of activity of all intensities: light, moderate, or vigorous intensity. This is the average amount of activity observed among children of this age and is consistent with guidelines from Canada, the United Kingdom, and the Commonwealth of Australia.
School-aged youth (ages 6 through 17 years) can achieve substantial health benefits by doing moderate and vigorous-intensity physical activity for periods of time that add up to 60 minutes or more each day. This activity should include aerobic activity as well as age-appropriate muscle- and bone-strengthening activities. It appears that, as in adults, the total amount of physical activity is more important for achieving health benefits than is any one component (frequency, intensity, or duration) or specific mix of activities (aerobic, muscle strengthening, bone strengthening).
Children and adolescents should meet the key guidelines by doing activities that are appropriate for their age. Their natural patterns of movement differ from those of adults. For example, children are naturally active in an intermittent way, particularly when they do unstructured active play. During recess and in their free play and games, children use basic aerobic and bone-strengthening activities, such as running, hopping, skipping, and jumping, to develop movement patterns and skills. They alternate brief periods of moderate- and vigorous intensity activity with periods of light-intensity physical activity or rest. Any episode of moderate- or vigorous intensity physical activity, however brief, counts toward the key guidelines for children and adolescents ages 6 through 17 years. For preschool-aged children, activity of any intensity counts, including light intensity.[8]
 |
REFLECTIVE PRACTICE
What were some of your favorite physical activities as a child? Why did you enjoy these? Are they included in Table 13.1? |
|---|
Table 13.1 – Examples of Physical Activities for Children[9]
| Type of Physical Activity | Preschool Aged Children | School Aged Children |
|---|---|---|
| Moderate-Intensity Aerobic |
|
|
| Vigorous-Intensity Aerobic |
|
|
| Muscle Strengthening |
|
|
| Bone Strengthening |
|
|

One practical strategy to promote activity in children is to replace sedentary behavior with activity whenever possible. For example, where appropriate and safe, families should walk or bicycle to school or the bus stop instead of riding in a car. Rather than only watching sporting events on television, children should participate in age-appropriate sports or games.
- Children who do not meet the key guidelines should slowly increase their moderate-to-vigorous physical activity in small steps and in ways that they enjoy. A gradual increase in the number of days and the time spent being active will help reduce the risk of injury.
- Children who meet the key guidelines should continue doing moderate-to-vigorous physical activity every day and, if appropriate, become even more active. Evidence suggests that even more than 60 minutes of activity daily may provide additional health benefits for school-aged youth.
- Children who exceed the key guidelines should maintain their activity level and vary the kinds of activities they do to reduce the risk of overtraining or injury.
- Children with disabilities are more likely to be inactive than those without disabilities. Families of children with disabilities should work with a health care professional or physical activity specialist to understand the types and amounts of physical activity appropriate for them. When possible, children with disabilities should meet the key guidelines. When they are not able to participate in the appropriate types or amounts of physical activities needed to meet the key guidelines, they should be as active as possible and avoid being inactive.
Nutrition Education
Lifelong eating habits are shaped during a child’s early years. Teachers of young children have a special opportunity to help children establish a healthy relationship with food and lay the foundation for sound eating habits. Nutrition education and activities help set children on the path to a healthful lifestyle. Providing nutritionally balanced meals and snacks and integrating nutrition education and healthy eating habits in the home and early childhood.
Nutrition education for preschoolers fosters children’s awareness of different types of foods and promotes exploration and inquiry of food choices. Lifelong habits with foods are developed during early childhood. Through nutrition education in preschool, teachers encourage children to include a wide variety of foods that provide adequate nutrients in their daily diet.
Through knowledge, children become aware of different foods and tastes, some of which are familiar and others that are new. As they explore various foods and food preparations, they develop likes and dislikes and begin to make choices based on preference. Both nutrition choices and self-regulation of eating—that is, eating when hungry, chewing food thoroughly, eating slowly, and stopping when full— involve decision-making skills.
As children begin to understand the concepts of food identification and categorizing, teachers may describe how specific foods help our bodies. Children may better understand the overall benefit of food in terms of it helping them grow, giving them energy to run and play, and helping them to become strong. As children begin to understand internal body parts, teachers can initiate discussion of more specific food benefits.
Children need to understand that various foods help the body in different ways and that some children have specific food allergies.
For those with allergies, certain foods are potentially harmful to them. Teachers should encourage tasting and eating a variety of foods to obtain adequate nutrients for growth and development. “Variety” may mean foods of different color, shape, texture, and taste.
As children gain an understanding of different foods, they can begin to categorize foods in other ways, such as by food groups (e.g., bread, fruits, meat) or the U.S. Department of Agriculture (USDA) MyPlate food guide for young children. MyPlate reflects the 2010 Dietary Guidelines and replaces the MyPyramid for Preschoolers. Every food is all right, but some foods help the body more than others; therefore, people may eat some foods more often than others. Food models, combined with visual aids such as the Food Pyramid49 and integration of the topic with daily nutrition activities (e.g., mealtime, snack time, cooking activities), can help children begin to understand that some foods are eaten more frequently than others.
Here are some things that teachers can do to help educate children about nutrition:
- Introduce many different foods.
- Recognize and accommodate differences in eating habits and food choices.
- Provide opportunities and encouragement in food exploration.
- Integrate nutrition with other areas of learning through cooking activities.
- Show children where food is produced.
- Set up special areas to represent nutrition-related environments, such as grocery stores, restaurants, open-air markets, food co-ops, and picnics.
- Integrate nutrition education with basic hygiene education.
- Model and coach children’s behavior by eating from the same menu and encouraging conversations during mealtimes.
- Encourage children to share information about family meals.
- Serve meals and snacks family-style.
- Encourage tasting and decision making.
- Provide choices for children.
- Offer a variety of nutritious, appetizing foods in small portions.
- Encourage children to chew their food well and eat slowly.
- Teach children to recognize signs of hunger.
- Discuss how the body uses food.

Children learn about food and develop food preferences through their direct experiences with food (i.e., handling, preparing, eating) and by observing the eating behaviors of adults and peers. The goal in preschool is that children will learn to eat a variety of nutritious foods and begin to recognize the body’s physical need for food (i.e., hunger and fullness).
Through modeling, repeated and various exposures to food, and social experiences, children begin to develop eating behaviors that can prevail throughout life.[10]
 |
REFLECTIVE PRACTICE
Reflect on how you will support children’s nutrition education. What will be most natural/easiest for you to do from this section? What might you have to be more intentional about (what might be more challenging or less natural)? |
|---|
Understanding Malnutrition
When children do not receive proper nutrition it affects their physical health and wellness. For many, the word “malnutrition” produces an image of a child in a third-world country with a bloated belly, and skinny arms and legs. However, this image alone is not an accurate representation of the state of malnutrition. For example, someone who is 150 pounds overweight can also be malnourished.
Malnutrition refers to one not receiving proper nutrition and does not distinguish between the consequences of too many nutrients or the lack of nutrients, both of which impair overall health. Undernutrition is characterized by a lack of nutrients and insufficient energy supply, whereas overnutrition is characterized by excessive nutrient and energy intake. Overnutrition can result in obesity, a growing global health threat.[11]
And if the cause of overnutrition is a diet that features food that is not nutrient-dense, a child could experience both overnutrition (too many calories) and undernutrition (inadequate micronutrients).
Undernutrition
Although not as prevalent in America as it is in developing countries, undernutrition is not uncommon and affects many subpopulations, including the elderly, those with certain diseases, and those in poverty.[12] Undernutrition is most often due to not enough high-quality food being available to eat. This is often related to high food prices and poverty. There are two main types of undernutrition: protein-energy malnutrition and dietary deficiencies.[13] Protein-energy malnutrition has two severe forms: marasmus (a lack of protein and calories) and kwashiorkor (a lack of just protein). Common micronutrient deficiencies include a lack of iron, iodine, and vitamin A.
Undernutrition encompasses stunted growth (stunting), wasting, and deficiencies of essential vitamins and minerals (collectively referred to as micronutrients).[14] Even moderate undernutrition can have lasting effects on children’s cognitive development. When children are hungry or undernourished, they have difficulty resisting infection and therefore are more likely than other children to become sick and to miss school. They are irritable and have difficulty concentrating, which can interfere with learning; and they have low energy, which can limit their physical activity. Some reports have estimated that millions of children in the United States experience hunger over the course of a year but no scientific consensus currently exists on how to define or measure hunger.[15] The term hunger, which describes a feeling of discomfort from not eating, has been used to describe undernutrition, especially in reference to food insecurity. [16]
Food Insecurity

Food insecurity is defined as the disruption of food intake or eating patterns because of a lack of money and other resources. In 2014, 17.4 million U.S. households were food insecure at some time during the year. Food insecurity does not necessarily cause hunger, but hunger is a possible outcome of food insecurity.
The United States Department of Agriculture (USDA) divides food insecurity into the following 2 categories:
- Low food security: “Reports of reduced quality, variety, or desirability of diet. Little or no indication of reduced food intake.”
- Very low food security: “Reports of multiple indications of disrupted eating patterns and reduced food intake.”
Food insecurity may be long term or temporary. It may be influenced by a number of factors including income, employment, race/ethnicity, and disability. The risk for food insecurity increases when money to buy food is limited or not available. In 2016, 31.6% of low-income households were food insecure, compared to the national average of 12.3%. children with unemployed parents have higher rates of food insecurity than children with employed parents. Racial and ethnic disparities exist related to food insecurity. In 2016, black non-Hispanic households were nearly 2 times more likely to be food insecure than the national average (22.5% versus 12.3%, respectively). Among Hispanic households, the prevalence of food insecurity was 18.5% compared to the national average (12.3%).
Neighborhood conditions may affect physical access to food. For example, people living in some urban areas, rural areas, and low-income neighborhoods may have limited access to full-service supermarkets or grocery stores. Predominantly black and Hispanic neighborhoods have fewer full-service supermarkets than predominantly white and non-Hispanic neighborhoods. Communities that lack affordable and nutritious food are commonly known as “food deserts.” Convenience stores and small independent stores are more common in food deserts than full-service supermarkets or grocery stores. These stores may have higher food prices, lower quality foods, and less variety of foods than supermarkets or grocery stores. Access to healthy foods is also affected by a lack of transportation and long distances between residences and supermarkets or grocery stores.[17]
Overnutrition
Overnutrition is a form of malnutrition (imbalanced nutrition) arising from excessive intake of nutrients, leading to an accumulation of body fat that impairs health (i.e., overweight/obesity).[18] Overnutrition is an epidemic in the United States and is known to be a risk factor for many diseases, including Type 2 diabetes, cardiovascular disease, inflammatory disorders (such as rheumatoid arthritis), and cancer.[19]
Overweight and Obesity in Childhood
Obesity means having too much body fat. It is different from being overweight, which means weighing too much. Both terms mean that a person’s weight is greater than what’s considered healthy for his or her height. Children grow at different rates, so it isn’t always easy to know when a child has obesity or is overweight.[20] Obesity is defined as a body mass index (BMI) at or above the 95th percentile of the CDC sex-specific BMI-for-age growth charts.[21]
In the United States, the percentage of children and adolescents affected by obesity has more than tripled since the 1970s. Obesity prevalence was 12.7% among 2- to 5-year-olds, 20.7% among 6- to 11-year-olds. Childhood obesity is also more common among certain populations.[22]
- Hispanic children (26.5%) and non-Hispanic Bleck children (24.8%) had higher obesity prevalence than non-Hispanic whites (16.6%).
- Non-Hispanic Asian children (9.0%) had lower obesity prevalence than non-Hispanic Black and Hispanic children.
Many factors contribute to childhood obesity, including:
- Genetics.
- Metabolism—how your body changes food and oxygen into energy it can use.
- Eating and physical activity behaviors.
- Community and neighborhood design and safety.
- Short sleep duration.
- Negative childhood events.
Genetic factors cannot be changed. However, people and places can play a role in helping children achieve and maintain a healthy weight. Changes in the environments where children spend their time—like homes, early care and education programs, schools, and community settings—can make it easier for children to access nutritious foods and be physically active. Early care and education programs and schools can adopt policies and practices that help young people eat more fruits and vegetables, eat fewer foods and beverages that are high in added sugars or solid fats, and increase daily minutes of physical activity.[23]
Nutrition Concerns During Childhood
To keep children well, it’s also important to be aware of common nutritional concerns during childhood. Two of those concerns are food allergies and intolerances and iron deficiency anemia.
Food Allergies and Food Intolerance
Food allergies impact four to six percent of young children in America. Common food allergens include peanuts, eggs, shellfish, wheat, and cow’s milk.[24] Recent studies show that three million children under age eighteen are allergic to at least one type of food.
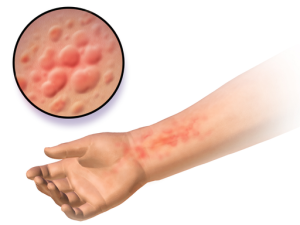
An allergy occurs when a protein in food triggers an immune response, which results in the release of antibodies, histamine, and other defenders that attack foreign bodies. Possible symptoms include itchy skin, hives, abdominal pain, vomiting, diarrhea, and nausea. Symptoms usually develop within minutes to hours after consuming a food allergen. Children can outgrow a food allergy, especially allergies to wheat, milk, eggs, or soy.
Anaphylaxis is a life-threatening reaction that results in difficulty breathing, swelling in the mouth and throat, decreased blood pressure, shock, or even death. Milk, eggs, wheat, soybeans, fish, shellfish, peanuts, and tree nuts are the most likely to trigger this type of response. A dose of the drug epinephrine is often administered via a “pen” to treat a person who goes into anaphylactic shock.
Some children experience a food intolerance, which does not involve an immune response. Food intolerance is marked by unpleasant symptoms that occur after consuming certain foods. Lactose intolerance, though rare in very young children, is one example. Children who suffer from this condition experience an adverse reaction to the lactose in milk products. It is a result of the small intestine’s inability to produce enough of the enzyme lactase, which is produced by the small intestine. Symptoms of lactose intolerance usually affect the GI tract and can include bloating, abdominal pain, gas, nausea, and diarrhea. An intolerance is best managed by making dietary changes and avoiding any foods that trigger the reaction.[25]
Caring for Children with Food Allergies
Staff who work in schools and early care and education (ECE) programs should develop plans for how they will respond effectively to children with food allergies. Although the number of children with food allergies in any one school or ECE program may seem small, allergic reactions can be life-threatening and have far-reaching effects on children and their families, as well as on the schools or ECE programs they attend. Any child with a food allergy deserves attention and the school or ECE program should create a plan for preventing an allergic reaction and responding to a food allergy emergency.
Studies show that 16%–18% of children with food allergies have reacted to accidentally eating food allergens while at school. In addition, 25% of the severe and potentially life-threatening reactions (anaphylaxis) reported at schools happened in children with no previous diagnosis of food allergy. School and ECE program staff should be ready to address the needs of children with known food allergies. They also should be prepared to respond effectively to the emergency needs of children who are not known to have food allergies but who exhibit allergic signs and symptoms.
The symptoms of allergic reactions to food vary both in type and severity among individuals and even in one individual over time. Symptoms associated with an allergic reaction to food include the following:
- Mucous Membrane Symptoms: red watery eyes or swollen lips, tongue, or eyes.
- Skin Symptoms: itchiness, flushing, rash, or hives.
- Gastrointestinal Symptoms: nausea, pain, cramping, vomiting, diarrhea, or acid reflux.
- Upper Respiratory Symptoms: nasal congestion, sneezing, hoarse voice, trouble swallowing, dry staccato cough, or numbness around mouth.
- Lower Respiratory Symptoms: deep cough, wheezing, shortness of breath or difficulty breathing, or chest tightness.
- Cardiovascular Symptoms: pale or blue skin color, weak pulse, dizziness or fainting, confusion or shock, hypotension (decrease in blood pressure), or loss of consciousness.
- Mental or Emotional Symptoms: a sense of “impending doom,” irritability, change in alertness, mood change, or confusion.
Children sometimes do not exhibit overt and visible symptoms after ingesting an allergen, making early diagnosis difficult. Signs and symptoms can become evident within a few minutes or up to 1–2 hours after ingestion of the allergen, and rarely, several hours after ingestion.
Children might communicate their symptoms in the following ways:
- It feels like something is poking my tongue.
- My tongue (or mouth) is tingling (or burning).
- My tongue (or mouth) itches.
- My tongue feels like there is hair on it.
- My mouth feels funny.
- There’s a frog in my throat; there’s something stuck in my throat.
- My tongue feels full (or heavy).
- My lips feel tight.
- It feels like there are bugs in there (to describe itchy ears).
- It (my throat) feels thick.
- It feels like a bump is on the back of my tongue (throat).
Some children may not be able to communicate their symptoms clearly because of their age or developmental challenges.
Emotional Impact on Children with Food Allergies and Their Families
The health of a child with a food allergy can be compromised at any time by an allergic reaction to food that is severe or life-threatening. Many studies have shown that food allergies have a significant effect on the psychosocial well-being of children with food allergies and their families.
Families of a child with a food allergy may have constant fear about the possibility of a life-threatening reaction and stress from constant vigilance needed to prevent a reaction. They also have to trust their child to the care of others, make sure their child is safe outside the home, and help their child have a normal sense of identity.
Children with food allergies may also have constant fear and stress about the possibility of a life-threatening reaction. The fear of ingesting a food allergen without knowing it can lead to coping strategies that limit social and other daily activities. Children can carry emotional burdens because they are not accepted by other people, they are socially isolated, or they believe they are a burden to others. They also may have anxiety and distress that is caused by teasing, taunting, harassment, or bullying by peers, teachers, or other adults. School and ECE program staff must consider these factors as they develop plans for managing the risk of food allergy for children with food allergies.
Food Allergy Management in Early Care and Education Programs
Early learning program staff should develop a comprehensive strategy to manage the risk of food allergy reactions in children. This strategy should include (1) a coordinated approach, (2) strong leadership, and (3) a specific and comprehensive plan for managing food allergies.
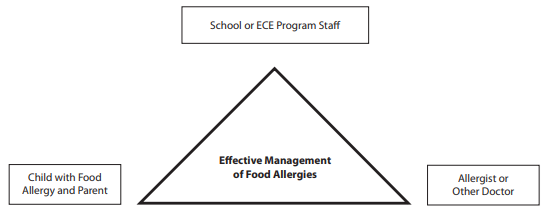
- Use a coordinated approach that is based on effective partnerships. The management of any chronic health condition should be based on a partnership among early learning program staff, children and their families, and the family’s allergist or other doctor.
- The collective knowledge and experience of a licensed doctor, children with food allergies, and their families can guide the most effective management of food allergies in schools or ECE programs for each child. Close working relationships can help ease anxiety among parents, build trust, and improve the knowledge and skill of school or ECE program staff members.
- Provide clear leadership to guide planning and ensure implementation of food allergy management plans and practices. This may be the administrator or the person that coordinates health services for children (health consultant, school nurse, etc.)
- Develop and implement a comprehensive plan for managing food allergies. To effectively manage food allergies and the risks associated with these conditions, many people inside and outside the school or ECE program must come together to develop a comprehensive plan, called the Food Allergy Management and Prevention Plan (FAMPP).
The FAMPP should address the following five priorities:
- Ensure the daily management of food allergies for individual children.
- Identify children with food allergies.
- Develop a plan to manage and reduce the risk of food allergy reactions in individual children, usually called a food allergy Emergency Care Plan (ECP). The ECP should be written by the child’s physician and confirmed with the parents. It should include:
- A recent photo of the child.
- Information about the food allergen, including a confirmed written diagnosis from the child’s doctor or allergist.
- Information about signs and symptoms of the child’s possible reactions to known allergens.
- Information about the possible severity of reactions, including any history of prior anaphylaxis (even though anaphylaxis can occur even in children without a history of prior anaphylaxis).
- A treatment plan for responding to a food allergy reaction or emergency, including whether an epinephrine auto-injector should be used.
- Information about other conditions, such as asthma or exercise-induced anaphylaxis that might affect food allergy management.
- Contact information for parents and doctors, including alternate phone numbers for notification in case of emergency
- Prepare for food allergy emergencies.
- Set up communication systems that are easy to use (intercoms, walkie-talkies, cell phones, etc.)
- Make sure staff can get to epinephrine auto-injectors quickly and easily
- Make sure that epinephrine is used when needed and someone immediately contacts emergency medical services
- Identify the role of each staff member in an emergency
- Prepare for food allergy reactions in children without a prior history of food allergies.
- Document the response to a food allergy emergency
- Provide professional development on food allergies for staff members.
- Provide general training on food allergies for all staff.
- Provide in-depth training for staff who have frequent contact with children with food allergies.
- Provide specialized training for staff who are responsible for managing the health of children with food allergies on a daily basis.
- Educate children and family members about food allergies.
- Teach all children about food allergies
- Teach all parents and families about food allergies.
- Create and maintain a healthy and safe educational environment.
- Create an environment that is as safe as possible from exposure to food allergens.
- Develop food-handling policies and procedures to prevent food allergens from unintentionally contacting another food.
- Make outside groups aware of food allergy policies and rules when they use school or ECE program facilities before or after hours.
- Create a positive psychosocial climate (one that prevents bullying, teasing, and harassing).
Early care and education programs are responsible for the health and safety of children with food allergies. Through the collective efforts of school and ECE program staff members, parents, and health care providers, children with food allergies can be assured a safe place to thrive, learn, and succeed.[26] When creating a plan to for food allergies like FAMPP, early learning programs need to ensure they are including what is required for addressing food allergies per WAC 110-300-0186.
 |
GLUTEN INTOLERANCE AND CELIAC DISEASE
One particular intolerance to be aware of that may affect children in early care and education programs is gluten intolerance. Gluten is a protein found in wheat, rye, and barley. It is found mainly in foods but may also be in other products like medicines, vitamins, and supplements. People with gluten sensitivity have problems with gluten. It is different from celiac disease (see below), an immune disease in which people can’t eat gluten because it will damage their small intestine.
Some of the symptoms of gluten sensitivity are similar to celiac disease. They include tiredness and stomachaches. It can cause other symptoms too, including muscle cramps and leg numbness. But it does not damage the small intestine like celiac disease.
Researchers are still learning more about gluten sensitivity.[27] A more serious concern surrounding gluten that has more acknowledgment in the medical field is celiac disease.
Celiac Disease Celiac disease is an immune disease in which people can’t eat gluten because it will damage their small intestine. If they have celiac disease and eat foods with gluten, the immune system responds by damaging the small intestine. Gluten is a protein found in wheat, rye, and barley. It may also be in other products like vitamins and supplements, hair and skin products, toothpaste, and lip balm.
Celiac disease affects each person differently. Symptoms may occur in the digestive system, or other parts of the body. One person might have diarrhea and abdominal pain, while another person may be irritable or depressed. Irritability is one of the most common symptoms in children. Some people have no symptoms.
Celiac disease is genetic. Blood tests and tissue biopsies may be used to diagnose celiac disease. 589 “Many kids are diagnosed with it when they’re between 6 months and 2 years old, which is when most kids get their first taste of gluten in foods.”[28] Treatment is a diet free of gluten, which is essential to prevent damage to the small intestine.[29] So it is critical that their food does not contain and is not contaminated with gluten. Because gluten is found in many foods, reading nutrition labels will be vital. Preparing food away from gluten containing food is also required to prevent cross-contamination. Gluten free versions of foods and gluten-free recipes will help early care and education staff (and families) to protect the nutritional well-being and health of children with celiac disease. |
|---|
Iron-Deficiency Anemia
Iron deficiency anemia is the most common cause of anemia in the United States.[30] This condition occurs when an iron-deprived body cannot produce enough hemoglobin, a protein in red blood cells that transports oxygen throughout the body. The inadequate supply of hemoglobin for new blood cells results in anemia. Iron-deficiency anemia causes a number of problems including weakness, pale skin, shortness of breath, and irritability. It can also result in intellectual, behavioral, or motor problems.
In infants and toddlers, iron-deficiency anemia can occur as young children are weaned from iron-rich foods, such as breast milk and iron-fortified formula. They begin to eat solid foods that may not provide enough of this nutrient. As a result, their iron stores become diminished at a time when this nutrient is critical for brain growth and development.
There are steps that parents and caregivers can take to prevent iron-deficiency anemia, such as adding more iron-rich foods to a child’s diet, including lean meats, fish, poultry, eggs, legumes, and iron-enriched whole-grain breads and cereals[31] and foods high in vitamin C, which helps the body absorb iron efficiently.[32] Although milk is critical for the bone-building calcium that it provides, intake should not exceed the recommended daily allowance (RDA) to avoid displacing foods rich with iron.[33]
Summary
Early care and education programs can create environments that protect children’s nutrition and physical wellness by following dietary guidelines and providing nutritious foods that appeal to children and keeping them active. It is important to understand forms of malnutrition that can affect families and children and to understand and plan for nutritional concerns that may affect children, such as food allergies and intolerances and iron deficiency anemia.
 |
Resources for Further Exploration
|
|---|
- Healthy Active Living: Tips for Health Managers by the National Center on Early Childhood Health and Wellness is in the public domain ↵
- Healthy Active Living: Tips for Health Managers by the National Center on Early Childhood Health and Wellness is in the public domain ↵
- Guidelines for School Health Programs to Promote Lifelong Healthy Eating by CDC Morbidity and Mortality Weekly Report (MMWR) is in the public domain ↵
- Healthy Active Living: Tips for Health Managers by the National Center on Early Childhood Health and Wellness is in the public domain ↵
- Khalsa, A. S., Kharofa, R., Ollberding, N. J., Bishop, L., and Copeland, K. A. (2017). Attainment of ‘5-2-1-0’ obesity recommendations in preschool-aged children. Preventive Medicine Reports, 8, 79–87. https://doi.org/10.1016/j.pmedr.2017.08.003 ↵
- Growing Healthy Family Goals Worksheet by Head Start Early Childhood Learning & Knowledge Center is in the public domain ↵
- Active Play: Tips for Families by the National Center on Early Childhood Health and Wellness is in the public domain ↵
- Physical Activity Guidelines for Americans, 2nd ed. by the U.S. Department of Health and Human Services is in the public domain ↵
- Physical Activity Guidelines for Americans, 2nd ed. by the U.S. Department of Health and Human Services is in the public domain ↵
- California Preschool Curriculum Framework (Volume 2) by the California Department of Education is used with permission ↵
- Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0 ↵
- Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0 ↵
- Malnutrition by Wikipedia is licensed under CC BY-SA 3.0 ↵
- Malnutrition by Wikipedia is licensed under CC BY-SA 3.0 ↵
- Guidelines for School Health Programs to Promote Lifelong Healthy Eating by CDC Morbidity and Mortality Weekly Report (MMWR) is in the public domain ↵
- Malnutrition by Wikipedia is licensed under CC BY-SA 3.0 ↵
- Food Insecurity by the Office of Disease Prevention and Health Promotion is in the public domain ↵
- Mathur, P., & Pillai, R. (2019). Overnutrition: Current scenario & combat strategies. The Indian Journal of Medical Research, 149(6), 695–705. https://doi.org/10.4103/ijmr.IJMR_1703_18 ↵
- Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0 ↵
- Obesity in Children by MedlinePlus is in the public domain ↵
- Childhood Obesity Facts by the Centers for Disease Control and Prevention is in the public domain ↵
- Childhood Obesity Facts by the Centers for Disease Control and Prevention is in the public domain ↵
- Childhood Obesity Facts by the Centers for Disease Control and Prevention is in the public domain ↵
- Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0 ↵
- Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0 ↵
- Voluntary Guidelines for Managing Food Allergies in Schools and Early Care and Education Programs by the Centers for Disease Control and Prevention is in the public domain ↵
- Gluten Sensitivity by MedlinePlus is in the public domain ↵
- del Rosario, J.F. (2015). Celiac Disease. Retrieved from https://kidshealth.org/en/kids/celiac.html ↵
- Celiac Disease by MedlinePlus is in the public domain ↵
- Guidelines for School Health Programs to Promote Lifelong Healthy Eating by CDC Morbidity and Mortality Weekly Report (MMWR) is in the public domain ↵
- Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0 ↵
- Guidelines for School Health Programs to Promote Lifelong Healthy Eating by CDC Morbidity and Mortality Weekly Report (MMWR) is in the public domain ↵
- Human Nutrition by University of Hawai‘i at Mānoa Food Science and Human Nutrition Program is licensed under CC BY 4.0 ↵

