Chapter 8 – Contraception
Learning Outcomes
- Analyze health, psychosocial, and cultural factors impacting contraception use.
- Discuss best practices to promote equity within healthcare systems and regarding access to resources.
- Be able to demonstrate the following in regard to contraception:
- ways in which sexual participants or partners can share responsibility for it;
- how various methods work as well as the advantages and disadvantages of each method;
- and finally, the effectiveness of various hormone-based contraceptives, barrier methods, intrauterine devices, emergency contraception, methods based on the menstrual cycle, and sterilization.
Introduction
One could argue that as long as humankind has had an awareness of how conception occurs, there have been steps taken to thwart that process. The history of contraception (the deliberate use of techniques to prevent pregnancy or sexually transmitted infections) is long and varied. In the United States, contraception is fraught with complexities. On one hand, there have been remarkable innovations, but on the other hand, there’s a sordid history of the mistreatment and forced sterilization of marginalized folks. This week’s reading attempts to highlight historical features of contraception, describe different types of contraception and how they work, and illuminate intersectional imbalances in access and delivery of contraceptive services.
Early History of Contraception – An Overview
As the old adage goes, “Necessity is the mother of invention” and, indeed, contraception is no exception to this rule. The first known record of contraception dates back to 3000 BCE and was the brainchild of Pasiphae, the wife of King Minos of Crete. Fearing that his semen had “serpents and scorpions” in it, she inserted a goat bladder into her vagina before having sex with her husband (Khan, Mukhtar, Dickinson, & Sriprasad, 2013). There’s also evidence in support of Ancient Greeks and Egyptians using a diaphragm made out of crocodile dung, honey, and sodium carbonate (Lehmiller, 2019; Tye, 2020) to prevent pregnancy. The Ancient Egyptians were one of the first civilizations to use barrier methods in the form of sheaths, often made out of linen while Chinese civilizations utilized silk paper applied with oil. Early Japanese civilization used a shell to cover the glans of the penis and the Djukas tribe of New Guinea are on record for using an internal condom made out of a specific plant, which prevented conception (Khan, et al, 2013; Lehmiller, 2019).
By the Renaissance, contraception was regarded as being both a safeguard from disease, as well as unintended pregnancy with condoms emerging with greater use (most were made from linen or animal intestines or bladders of goats, sheep, cattle, or fish). From Ancient cultures to the Renaissance and forward, the wisdom of herbs, teas and tinctures were also passed down from woman to woman. The popular ballad, “Scarborough Fair” was thought to hold the secret to avoiding pregnancy through the use of parsley, sage, rosemary and thyme and pennyroyal tea was commonly used as an abortifacient (Bilger, 1998). By the middle to late 19th century condoms and investigations to hormonal contraceptives were underway, paving the way for 20th and 21st century innovation and use.
Types of Contraceptives
Behavioral Methods
In early lore, behavioral techniques to prevent pregnancy were often based on superstition or storytelling. For example, women were often instructed to jump up and down to get rid of the semen in their vagina or to sneeze or cough heartily (Lehmiller, 2019). Unsurprisingly, these methods weren’t very effective. Perhaps the most successful form of contraception is abstinence and, indeed, its virtue has been touted for generations. Although, theoretically, abstinence emerges as the most cost effective and reliable form of contraception, it’s not always the most attainable or realistic. In cases where sexual intercourse is likely to occur but where accessibility to contraception is limited or religiosity forbids certain forms of protection, behavioral methods are often employed. These methods are typically designed to reduce the chance of conception versus STI prevention.
In the United States, there are over 61 million women who fall within reproductive age (15-44) and about 70% of them are at risk for unintended pregnancy (Guttmacher Institute, 2020). Importantly, 99% of women within this age group disclosed using at least one contraceptive method with over 10% using a behavioral method (Guttmacher Institute, 2020). One of the most commonly known behavioral methods of contraception is the withdrawal method in which the penis is withdrawn from the vagina before ejaculating. Unfortunately, this method is the least effective form of birth control since sperm may be released in pre-ejaculate, it can enter via contact with labia or clitoris, and/or because timing of the withdrawal isn’t done before ejaculation. Indeed, research notes that over a quarter of women (27%) using this method will become pregnant within a year (Tye, 2020).
Timed abstinence, or the rhythm method, is another common behavioral strategy. This approach utilizes reliance of menstrual cycle tracking with avoidance of sex during ovulation. Again, its efficacy is compromised when there are variation of implementation. Additionally, even with more technological advances in tracking menstrual cycles (period apps, ease of temperature recording, etc), physiological variations (like irregular periods) can reduce this method’s efficacy.
Finally, another behavioral contraceptive method that is very specific to certain situations involves breastfeeding. Indeed, intensive breast-feeding (6-8 times per day) can aid in suppressing ovulation. This results in a physiologically based contraception, with only 2% of women becoming pregnant within the year. There are contrary data regarding how long this method is effective with some research supporting six months while other supports nine months postpartum (Tye, 2020).
One behavioral method that isn’t often discussed, in part because of continued taboos about the behavior, is sex during menstruation. It’s actually more common than one may realize (some like the additional lubrication and/or the spike in arousal), while others may be averse to the idea. To be clear, sex during menstruation is completely safe (do watch for STI prevention, however). Importantly, sex on your period in NOT a contraceptive strategy. Indeed, because some sperm can live up to a week and because some menstrual cycles are irregular, pregnancy can still occur so additional contraception may be needed (Tye, 2020).
Barrier Methods
Earlier we discussed how evidence of barrier methods, be it a condom or a diaphragm, appeared in ancient civilizations. By the time we reach mid-late 19th century, significant advances were made, and in 1860, condoms were produced on a large scale. In part, this was because the vulcanized rubber introduced by Charles Goodyear (yep- the tire guy) changed the ability to mass produce condoms (versus relying on animal products). Originally, rubber condoms were made to scale and were reusable (Khan, et al, 2013). Unfortunately, U.S. Postal Inspector and secretary of the New York Society for the Suppression of Vice, Anthony Comstock, lobbied for the prohibition of any type of advertising or print materials involving contraception. In 1873, the Comstock Act was passed, making it a federal offense to disseminate contraceptive information and, ultimately, a series of “Comstock Laws” were implemented nationwide, resulting in the criminalization of contraceptive use (Bailey, 2010).
In 1920, the invention of latex reshaped condom production. During World Wars I and II, rates of STIs among American soldiers skyrocketed and distribution of condoms finally appeared on scene during WW II. Post-war attitudes toward contraception started to shift in the late 1940s (Khan, et al, 2013). Still, it wasn’t until 1965, in the Supreme Court decision on Griswold vs. Connecticut that attitudes and accessibility of contraception takes a dramatic shift toward legality and acceptance (Bailey, 2010).
The most commonly used barrier method in the United States is the male condom (Copen, 2017; Daniels & Abma, 2018). According to the Guttmacher Institute (2020), 5.5 million women rely on male condoms for their contraception needs, making it the most common among 15 to 19 year olds, those born outside of the U.S. and uninsured college graduates (and a few others). While condom use is the most efficacious in the prevention of STIs, its use in pregnancy prevention yields more variable results.
With perfect use, condoms have a 98% efficacy rate in preventing pregnancy. However, that number declines to 82% when human error is factored in (Lehmiller, 2019). The most common mistakes with condom use is not using them correctly, not using them each time intercourse occurs, and breakage (Tye, 2020). Other issues include failing to withdraw promptly after ejaculation, using latex-incompatible lubricant (remember not to mix oil-based lube with latex), and reusing condoms (Lehmiller, 2019).
Other barrier methods include the internal condom (sometimes called the female condom) and cervical barriers, such as the diaphragm and cervical cap. The internal condom is typically made out of polyurethane (versus latex) and is a hollow closed cylinder with an outer and an inner ring. The inner ring fits close to the cervix, while the out ring remains outside the labia (some report enjoying the extra clitoral stimulation). If the inner ring is removed, it can also be used for anal sex. Available widely throughout Europe, the internal condom can be obtained in the US by prescription, online, or through some reproductive health clinics (Lehmiller, 2019; Tye, 2020). When it’s used as a female condom and barring any errors, the internal condom is believed to be as effective as the male condom in preventing pregnancy and STIs. Unfortunately, the internal condom is a bit more complicated, resulting in less efficacy (Tye, 2020).
The diaphragm and cervical cap are both designed to be inserted into the vagina before sexual intercourse (and typically with the addition of spermicide). Once quite popular in the United States, this is one of the least common forms of contraception today. Still, it is cost-effective (a diaphragm or cervical cap can last up to a year) but it does require fitting it to your particular cervix and a comfort in insertion before sex. Additionally, they need to be left in the body six hours post intercourse to ensure protection. When used without error, the effectiveness of preventing pregnancy is up to 96%, though 88% effective with typical use (Lehmiller, 2019). For more information comparing and contrasting barrier methods of contraception, check out the Center for Disease Control or Planned Parenthood website.
Hormonal Contraception
Historical Notes
Similar to barrier methods, the history of hormonal contraception has a complex and varied background. As previously discussed, there was a range of contraceptive practices used by people for hundreds of years. Despite some informational and technological advances, the Comstock Act of 1873 reduced access and knowledge regarding contraception throughout the United States. One of the most critical opponents of Comstock laws was Margaret H. Sanger (1879 – 1966). A suffragette and advocate for social reform, Sanger argued that a woman’s right to control her body was a fundamental human right and that every person should be able to decide when and whether they should have a child. As a nurse she began speaking and writing about women’s reproductive health, ultimately being held in contempt for violating the Comstock Act in 1912.
In attending poverty-stricken patients from the Lower East Side of New York, she was overwhelmed with the lack of options for women desperate to limit their pregnancies. Following the tragic loss of one mother who died from a self-induced abortion, Sanger left nursing to advocate for women’s birth control later that year. A constant target of law enforcement officials keen on prosecuting Sanger for her work, she consistently moved forward with advocacy and education, ultimately creating the American Birth Control League in 1921 (which later became the Planned Parenthood Federation of America). Ultimately, Sanger’s work helped bring about the reversal of federal and state ‘Comstock laws’ and pioneered the medical efforts of the birth control pill (Nunez-Eddy & Malladi, 2016; 2018; Planned Parenthood, 2016; Tye, 2020).
As pioneering and innovative as Margaret Sanger was, there were also racist and ableist attitudes of the time that impacted her advocacy. A number of sources have noted her alignment with eugenicist thinking (the notion of selective ‘breeding’ to reinforce more favorable traits). Indeed, the birth control pill was created in response to difficulties with family planning and population control. After the Great Depression, when poverty was a serious problem throughout the nation, smaller families were seen as an affordable way to tackle poverty.
Since eugenics promoted the reproduction of only the healthiest (and let’s face it… the whitest) offspring, the implications of prejudice are abhorrent. Unfortunately, during the time the eugenics movement was popularized, it influenced Sanger and the ideas of birth control (Buttar & Seward, 2009; 2018). To her credit, she never reinforced the notion of sterilization, as did other eugenicists (Nunez-Eddy & Malladi, 2016), but it’s critical to evaluate all aspects of this notable figure versus glamorizing or ignoring elements of her advocacy that may have been problematic. Because, there is no question that aspects of ableism and racism are to be repudiated. For a more thorough response to criticism of Sanger’s perspective, please read Planned Parenthood’s statement on this.
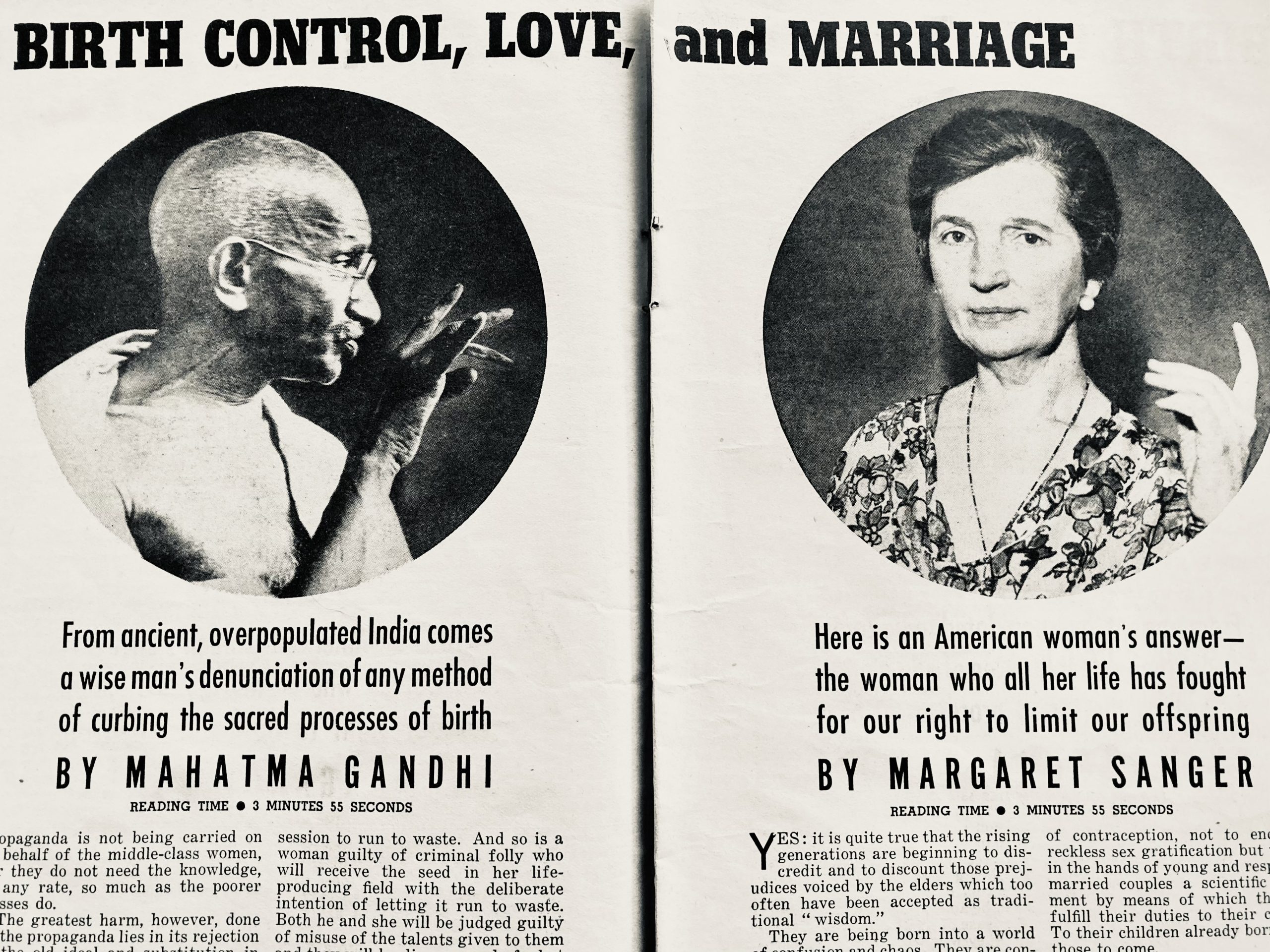
Image from Liberty Magazine, circa 1939
Because of Sanger’s advocacy and the efforts of many other individuals, groups, and corporations, the first commercial birth control pill, Enovid, was introduced, publicly, in 1960 (Bailey, 2010; Buttar & Seward, 2009; 2018). Marketed specifically for married couples, some states still banned the sale of contraception due to the last hold of Comstock provisions throughout the country. In 1965, the Supreme Court ruled in Griswold vs. Connecticut that married couples had the right to privacy in terms of contraception (opening up the sale and distribution of contraceptive items, including the pill; Bailey, 2010; Tye, 2020). In 1972, a second Supreme Court case, Eisenstadt vs. Baird extended contraceptive protections to unmarried women (Tye, 2020). The accessibility of birth control, combined with various cultural shifts, were instrumental in moving women’s rights forward in remarkable ways (Bailey, 2010; Tye, 2020).
Oral Contraceptives
There are several forms of hormonal contraception to discuss. Importantly, these interventions are primarily used for menstrual cycle care and/or to prevent unintended pregnancies (defined as mistimed and/or unwanted pregnancies; Jackson, Wang, & Morse, 2017). The birth control pill (also known as oral contraceptives) is the second most common form of contraception globally (Guttmacher Institute, 2020) and the most commonly prescribed contraceptive in the United States (Cooper & Mahdy, 2020). Approximately four out of five sexually active women have used the pill (though numbers are shifting based on availability of other hormonal options; Guttmacher Institute, 2020).
There are three different oral contraceptive options; combined estrogen-progesterone (most commonly prescribed), progesterone only and the continuous or extended use pill (Cooper & Mahdy, 2020; Lehmiller, 2019; Tye, 2020). When used perfectly, that is taken at the same time, everyday, with no deviation, the efficacy of the pill is 98-99%. However, typical use, which accounts for human error, failure rate for oral contraception is 9% (Cooper & Mahdy, 2020). For more on the types of oral contraceptive options, please check out the CDC and Planned Parenthood.
As revolutionary as the birth control pill has been, it is not without its challenges, as many users can attest to. There are wide-range of side-effects of taking oral contraceptives that have been reported in the 60+ years of its existence. In addition to changes in menstrual cycle, potential for spotting between periods, cramping, nausea, vomiting, weight loss, weight gain, sleep change and shifts in bone density, evidence also supports changes in mood, changes in sexual attraction and libido, increase in anxiety symptoms, shifts in emotion regulation and detection, stress response changes, and mixed data about both increased and decreased levels of cognitive functioning Cooper & Mahdy, 2020; de Wit, Booij, Giltay, Joffe, Schoevers, & Oldehinkel, 2020; Hill, 2020; Lehmiller, 2019; Lewis, Kimmig, Zsido, Jank, Derntl, & Sacher, 2019; Pahnke, Mau-Moeller, Junge, Wendt, Weymar, Hamm, & Lischke, 2019). These are all areas for continued exploration, elaboration, and intervention, especially as symptoms may affect marginalized communities differently and deleteriously.
Other Hormonal Contraceptive Options
There are two other types of hormonal contraceptives to be aware of. First, there are hormonal interventions that have various compositions similar to the variety of oral contraceptives. The primary difference is the form of modality since these hormonal contraceptives are delivered through injection (e.g. Depo-Provera, administered once every three months), transdermal patches (e.g. Ortho Evra, administered once a month) or a vaginal ring (e.g. NuvaRing, placed vaginally once a month; Lehmiller, 2019; Planned Parenthood, 2020, Tye, 2020).
The other hormonal contraceptive category is long-acting reversible contraceptives (LARC). One of these options is administered through an implant (administered under the skin of the upper arm), lasts for five years and has an efficacy rate of 99%. There’s also the placement of an intrauterine device (IUD), which once placed can last for 3 to 12 years, making it one of the most convenient options for long-term pregnancy prevention.
Perhaps the biggest change in the use of hormonal contraceptives is the increase in the use of LARCs. The new options available to women has seen widespread adoption among all ages and races. LARC use was highest among women aged 25-34 (as compared to other age ranges from 15 to 49; Daniels & Abma, 2018; Guttmacher Institute, 2020). The proportion of women who have used the injectable method increased from 5% in 1995 to 23% in 2006–2010 (Guttmacher Institute, 2020). Approximately 9% of Latina women are using LARC methods as compared to 7% of white and 5% of black users (Jackson, Wang, & Morse, 2017).
Important Considerations
Gaining access to hormonal contraception remains a significant issue, negatively impacting marginalized communities (minorities, economically disadvantaged, immigrants, disabled, etc). Indeed, the majority of oral contraceptive users are white, young, childless, and college educated (Guttmacher Institute, 2020). White women use the pill more often (19%) compared to Latina and black women (11% and 10% respectively). Although there has been a decline of unintended pregnancies across all racial groups, 45% in 2011 compared to 51% in 2008, the racial differences have remained fixed with blacks and Latinas experiencing higher rates than white women (even when stratified by income; Jackson, Wang, & Morse, 2017; Rocca & Harper, 2012; Wright, 2020).
Many of the disparities rooted in structural racism, which impacts minority women also impact women with disabilities. Among American women who fall within the reproductive age range, 12 to 18 percent have a disability related to mobility, vision, hearing, cognitive functioning and/or independent living. Unfortunately, women with disabilities are often subjected to healthcare bias and deemed asexual, which is not rooted in the experience of many these women. Multiple studies have shown that disabled women are less likely to receive gynecological exams and/or contraceptive counseling (Horner-Johnson, Akobirshoev, Amutah-Onukagha, Slaughter-Acey, & Mitra, 2021).
An additional area of consideration for contraceptive counseling, access, and patient-centered care is in the responsiveness to transgender and gender-diverse people. With approximately one in 200 adults identifying as transgender, this domain of care is essential to update. In one study of 26 transgender men, half were at risk for unintended pregnancy (Cipres, Seidman, Cloniger, Nova, O’Shea, & Obedin-Maliver, 2017). Importantly, evidenced-based care, which includes a patient-centered approach, is of paramount importance since each transmasculine or gender diverse patient has their own unique set of goals and concerns in terms of their reproductive health (Bonnington, Dianat, Kerns, Hastings, Hawkins, De Haan, & Obedin-Maliver, 2020).
In the examination of intersectional identities and contraceptive use, a few important findings come to light. First – there is consistent evidence that Black, Latina, Native American, Pan-Asian, disabled, gender diverse and poor women experience barriers to contraceptive access, have higher rates of contraceptive failure, and increased risks of adverse outcomes (Horner-Johnson, et al, 2021; Jackson, Wang, & Morse, 2017; Wright, 2020).
Secondly, practitioners of all types should acknowledge the history of inequity and structural racism, generally and as it pertains to contraceptive access since it still has a residual impact on women to this day.
Finally, there is an increased need to address women’s intersectional identities in response to their contraceptive needs, taking into account historical injustices and current, systemic inequities. As Kelsey Wright contends in her paper refuting the idea that contraception is a panacea for poverty reduction, “…contraceptive services should be offered to women in ways that ensure access to reproductive justice without obscuring the need for social changes in the institutions that create disadvantages and shape contraceptive use itself” (Wright, 2020, p. 1).
Sterilization
The final form of contraception to discuss is sterilization, an irreversible form of birth control that is the most commonly used in the United States and globally (Daniels & Abma, 2018; Guttmacher Institute, 2020). Typically applied to folks on the older end of the reproductive spectrum (ages 35-44) who have already had children, there are two kinds of sterilization to know. Female sterilization, or tubal ligation (tubectomy), is the process of clamping or severing the fallopian tubes so that any eggs released cannot meet sperm for fertilization. Male sterilization occurs in the form of a vasectomy, which involves the sealing or severing of the vas deferens so that sperm can no longer be in the ejaculate. Note that sperm is only a tiny fraction of seminal fluid so the difference in ejaculate is typically undetectable. Both of these procedures are considered low risk, 99% effective and cause no impairment in sexual functioning (Lehmiller, 2019; Tye, 2020).
Forced Sterilization as a Form of Racism
Although sterilization is a sound and viable option for many people in terms of contraception, there are some inequities in terms of who receives sterilization, which is born from a sordid history of coerced and forced sterilization. Summarized in Guttmacher Institute (2020) report, sterilization “is most common among blacks and Hispanics, women aged 35 or older, ever-married women, women with two or more children, women living below 150% of the federal poverty level, women with less than a college education, women living outside of a metropolitan area, and those with public or no health insurance” (p. 2). When considering issues of contraceptive decision making with minority and underrepresented women, listening and understanding their potential distrust in medical systems is essential (Horner-Johnson, et al, 2021; Jackson, Wang, & Morse, 2017; Wright, 2020).
In the mid-19th century, the eugenics movement, spearheaded by Sir Francis Galton, advocated for the advancement of promising heritability. By the late 1800s this campaign endorsed the elimination of hereditary “blights” such as non-whiteness, ‘feeble-mindedness,’ physical impairments or criminality. The United States was the first nation to enact laws of forced sterilization and in 1907, the state of Indiana allowed and/or required the sterilization of criminals, the intellectually disabled (ID) and institutionalized people with other mental and physical impairments. Other states soon followed and in 1927, the case Buck vs. Bell was struck down by the US Supreme Court (SCOTUS), ensuring the constitutionality of forced sterilization. The lawsuit had been filed by Virginia woman, Carrie Buck, who was forcibly sterilized and deemed unfit due to her ‘feeble-mindedness.’ The SCOTUS ruling all but ensured the continuation of negative eugenics throughout the country for decades to come (Amy & Rowlands, 2018; Asbury, 2015; Stern, 2005).
Films on Demand Video Clip: ‘Ann Cooper Hewitt’ – From Title:The Eugenics Crusade
When World War II came to an end, there was a collective, global outrage at the atrocities committed by the Nazis (who were well-documented to have learned a great deal from American eugenics). The presence of eugenics in the United States was no longer as heartily supported. Unfortunately, there was little to no change in the legality and practice of eugenics; simply a shift in the framing of the practice. Indeed, by the mid-20th century, tens of thousands of forced sterilizations had occurred in at least 32 states (with a third of those coming from California, alone; predominantly on poor black and Latina women; Stern, 2005). The states of Virginia and North Carolina had alarmingly high rates, dramatically impacting poor, black women (Amy & Rowlands, 2018; Asbury, 2015).
By the 1960s, forced sterilization started to take a different shape, shifting from the public health concerns of heritability issues to a form of public welfare. With the rise of contraceptive availability, sterilizations were seemingly ‘voluntary,’ however, frequently women did not have all of the information, were required to agree to sterilization in order to receive federal benefits, were coerced or simply lied to about the nature of the procedure. A devastating example of this emerged in the late 60s when it was publicized that 35% of all Puerto Rican women (ages 20-49) were sterilized (Krase, 2014).
In 1973, the Relf sisters gained notoriety among activists because at the ages of 12 and 14 they were forcibly sterilized in the state of Alabama. Their mother thought she was consenting to a reversible procedure and was threatened with the loss of her public benefits if she did not sign. In the federal lawsuit, the judge ruled in their favor, noting that “an indefinite number of poor people have been improperly coerced into accepting a sterilization operation under the threat that variously supported welfare benefits would be withdrawn unless they submitted” (as cited in Stern, 2015, p. 7).
Similar experiences for other minority groups were going on throughout the country. During the 60s and 70s, Native American women were especially at risk. About 40% (60,000–70,000) of all Native American women alive at that time, and 10% of Native American men underwent sterilization during the 1970s (Amy & Rowlands, 2018, p. 126; Blakemore, 2016). In 1979, Mexican American women in California filed a federal lawsuit, Madrigal v Quilligan, due to the forcible, coercive “consent” to sterilization. Almost all of the victims were in the midst of a painful, complex birthing process and were only given medication if they consented to the sterilization procedure. Unfortunately, they did not win their case, as the federal judge ruled in favor of the attending physicians (since they meant no harm). Still – the case garnered attention and effected changes in the formulation of sterilization stipulations (e.g. need to provide bilingual consent forms; Stern, 2015).
Under the guise of family planning, coercive sterilization was still an issue in the late 20th century, still predominantly affecting minority women. By 1983, forty-three percent of women sterilized in federally funded family planning programs were black (when blacks only made up 12% of the general population; Asbury, 2015). In the 90s, linking more experimental contraceptive options, like Norplant, were also connected to benefits for disadvantaged women. As Asbury (2015) wrote, “What is here worth noting is that the targeting of coercive contraception to poor, black women is antithetical to promoting their reproductive freedom and should be understood as a modern manifestation of historical eugenic efforts seeking to discourage reproduction by marginalized populations” (p. 13).
Current Issues
Unfortunately, coercive and forced sterilization in the United States is still happening. In September 2020 (just a short time ago), whistleblower and nurse Dawn Wooten, who worked at the Irwin County Detention Center (ICDC) in Georgia, shared that ICE detained women were being transferred to a physician who sterilized them without proper informed consent. In her complaint, Wooten also described multiple forms of medical abuse, from failures to protect patients against COVID-19, to forced hysterectomies (Manian, 2020).
Is it any wonder that, based on rampant, systemic injustice against many marginalized bodies that underrepresented folks are still cautious about contraceptive counseling? Indeed, there’s so much to rectify in terms of reproductive healthcare. Recognizing and reconciling the United States’ abhorrent practices is part of the process. Providing restitution and remedy for those deeply impacted, presently and historically, can certainly serve as another part of the solution. Finally, enacting, implementing, and enforcing reproductive rights policy that protects our most vulnerable citizens is certainly an essential feature, as well.
Conclusion
The innovation and use of contraceptive devices have a long, complex history. On one hand, our creative ingenuity can empower options to care for reproductive processes in really responsive ways. On the other hand, certain contraceptive practices are marred with abuse and exploitation, which has continued implications in reproductive justice. Thankfully, modern processes can afford us continued opportunities to correct past mistakes, ensure present accessibility and accountability, and innovate for diverse, responsive future options.
Licenses & Attributions
All Rights Reserved
Hill, S. E. (2019, December 2). The surprising link between women’s brains and the birth control pill. TEDxVienna. https://www.youtube.com/watch?v=RdwLAyWHBVs. License: All Rights Reserved. License Terms: Standard YouTube license.
Planned Parenthood (2019, July 19). What is an IUD? Learn about IUD effectiveness [Video]. https://www.youtube.com/watch?v=Aomv80RexVo&t=2s. License: All Rights Reserved. License Terms: Standard YouTube license.
Vlog Brothers (2017, July 21). On condom failure. [Video]. https://www.youtube.com/watch?v=Z4dO_K_DufQ. License: Published under Creative Commons Attribution 3.0 license directly on YouTube.
References
Amy, J. J., & Rowlands, S. (2018). Legalised non-consensual sterilisation–eugenics put into practice before 1945, and the aftermath. Part 1: USA, Japan, Canada and Mexico. The European Journal of Contraception & Reproductive Health Care, 23(2), 121-129. http://eprints.bournemouth.ac.uk/30553/3/Forced%20sterilisation-Part%201%20Final.pdf
Asbury, B. D. (2015). Backdoor to eugenics-The risks of prenatal diagnosis for poor, black women. Duke Journal of Gender Law & Policy, 23, 1. https://scholarship.law.duke.edu/cgi/viewcontent.cgi?article=1300&context=djglp
Bailey, M. J. (2010). “Momma’s got the pill”: How Anthony Comstock and Griswold v. Connecticut shaped US childbearing. American Economic Review, 100(1), 98-129.
Bilger, B. (1998). The secret garden. Sciences, 38(1), 38-43. https://libproxy.pcc.edu/login?url=https://www.proquest.com/scholarly-journals/secret-garden/docview/212676114/se-2?accountid=8042
Blakemore, E. (2016). The little-known history of the forced sterilization of Native American women. JSTOR Daily. https://daily.jstor.org/the-little-known-history-of-the-forced-sterilization-of-native-american-women/
Bonnington, A., Dianat, S., Kerns, J., Hastings, J., Hawkins, M., De Haan, G., & Obedin-Maliver, J. (2020). Society of Family Planning clinical recommendations: Contraceptive counseling for transgender and gender diverse people who were female sex assigned at birth. Contraception, 102(2), 70–82. https://doi.org/10.1016/j.contraception.2020.04.001
Buttar, A. & Seward, S. (2009). Enovid: The first hormonal birth control pill. Embryo Project Encyclopedia. http://embryo.asu.edu/handle/10776/1956.
Centers for Disease Control & Prevention (2020). Contraception. Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion. https://www.cdc.gov/reproductivehealth/contraception/index.htm#Contraceptive-Effectiveness
Cipres, D., Seidman, D., Cloniger III, C., Nova, C., O’Shea, A., & Obedin-Maliver, J. (2017). Contraceptive use and pregnancy intentions among transgender men presenting to a clinic for sex workers and their families in San Francisco. Contraception, 95(2), 186-189.
Cooper D. B. & Mahdy, H. (2020). Oral contraceptive pills. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430882/
Copen, C. E. (2017). Condom use during sexual intercourse among women and men aged 15-44 in the United States: 2011-2015 National Survey of Family Growth. National Health Statistics Reports, (105), 1-18. https://www.cdc.gov/nchs/data/nhsr/nhsr105.pdf
Daniels, K., & Abma, J. C. (2018). Current contraceptive status among women Aged 15–49: United States, 2017–2019. NCHS Data Brief, no 327. https://www.cdc.gov/nchs/data/databriefs/db327-h.pdf
de Wit AE, Booij SH, Giltay EJ, Joffe H, Schoevers RA, Oldehinkel AJ. (2020). Association of use of oral contraceptives with depressive symptoms among adolescents and young women. JAMA Psychiatry, 77(1):52–59. doi:10.1001/jamapsychiatry.2019.2838
Films Media Group. (2018). The eugenics crusade. Films On Demand. https://fod.infobase.com/PortalPlaylists.aspx?wID=105634&xtid=203114.
Guttmacher Institute (2020). Contraceptive use in the United States [Fact Sheet]. https://www.guttmacher.org/fact-sheet/contraceptive-use-united-states#
Hill, S. E. (2020). Feel like a different person on the pill? Here’s how it affects your mood. Ideas.TED. Retrieved from https://ideas.ted.com/how-the-birth-control-pill-affects-your-mood/
Horner-Johnson, W., Akobirshoev, I., Amutah-Onukagha, N. N., Slaughter-Acey, J. C., & Mitra, M. (2021). Preconception health risks among US women: Disparities at the intersection of disability and race or ethnicity. Women’s Health Issues, 31(1), 65-74.
Jackson, A. V., Wang, L. F., & Morse, J. (2017, August). Racial and ethnic differences in contraception use and obstetric outcomes: a review. Seminars in Perinatology, 41(5). 273-277.
Khan, F., Mukhtar, S., Dickinson, I. K., & Sriprasad, S. (2013). The story of the condom. Journal of the Urological Society of India, 29(1), 12–15. https://doi.org/10.4103/0970-1591.109976
Lehmiller, J. J. (2019). The psychology of human sexuality, 2nd edition. John Wiley & Sons, Ltd.
Lewis, C. A., Kimmig, A. C. S., Zsido, R. G., Jank, A., Derntl, B., & Sacher, J. (2019). Effects of hormonal contraceptives on mood: A focus on emotion recognition and reactivity, reward processing, and stress response. Current Psychiatry Reports, 21(11), 115.
Manian, M. (2020). Immigration detention and coerced sterilization: History tragically repeats itself. ACLU News & Commentary. https://www.aclu.org/news/immigrants-rights/immigration-detention-and-coerced-sterilization-history-tragically-repeats-itself/
Nunez-Eddy, C. & Malladi, L. (2016; 2018). Margaret Higgins Sanger (1879-1966). Embryo Project Encyclopedia http://embryo.asu.edu/handle/10776/11365.
Pahnke, R., Mau-Moeller, A., Junge, M., Wendt, J., Weymar, M., Hamm, A. O., & Lischke, A. (2019). Oral contraceptives impair complex emotion recognition in healthy women. Frontiers in Neuroscience, 12, 1041.
Planned Parenthood (2020, July 24). Statement about Margaret Sanger and Planned Parenthood’s mission. Retrieved from https://www.plannedparenthood.org/planned-parenthood-north-central-states/about-ppncs/media-relations/statement-about-margaret-sanger-and-planned-parenthoods-mission
Planned Parenthood (2021). Birth control. https://www.plannedparenthood.org/learn/birth-control
Rocca, C. H., & Harper, C. C. (2012). Do racial and ethnic differences in contraceptive attitudes and knowledge explain disparities in method use?. Perspectives on Sexual and Reproductive Health, 44(3), 150-158.
Stern, A. M. (2005). Sterilized in the name of public health: race, immigration, and reproductive control in modern California. American Journal of Public Health, 95(7), 1128-1138. https://ajph.aphapublications.org/doi/pdfplus/10.2105/AJPH.2004.041608
Tye, M. (2020). Sexuality and our diversity: Integrating culture with the biopsychosocial. Flatworld.
Wright, K. Q. (2020). Contraceptive selection and practice: Associations with self-identified race and socioeconomic disadvantage. Social Science & Medicine, 266, 113366.

