Several complications may occur during pregnancy, labor, delivery, and postpartum.
Complications of Pregnancy
There are several complications that can occur during pregnancy that pose health risks to mother and child. Common complications include the following[1]:
- Gestational diabetes (jĕs-TĀ-shŏn-ăl dī-ă-BĒ-tĭs): High blood sugar levels that develop in a woman during pregnancy who has not been previously diagnosed with diabetes. After pregnancy, blood sugars typically return to normal although the mother has increased risk of developing type 2 diabetes mellitus later in life.
- Hyperemesis gravidarum (HĪ-pĕr-ĕm-Ē-sĭs GRAV-ĭ-dar-ŭm): Severe, persistent vomiting during pregnancy causing dehydration and weight loss. It is more severe than nausea associated with “morning sickness.”
- Preeclampsia (prē-ĕ-KLAMP-sē-ă): High blood pressure during pregnancy with additional signs like edema and protein in the urine. If not effectively treated, preeclampsia can evolve into eclampsia (ĕ-KLAMP-sē-ă), severe complication characterized by seizures and a risk of coma and death.
- Deep vein thrombosis (dēp vān throm-BOH-sĭs): The formation of a blood clot in a deep vein, most commonly in the legs.
- Postpartum hemorrhage (pōst-PÄR-tŭm HEM-ŏr-ij): Cumulative blood loss greater than 1,000 mL with signs and symptoms of hypovolemia within 24 hours of the birth process, regardless of the route of delivery. Hypovolemia (hī-pō-vō-LĒ-mē-ă) is a life-threatening condition where the plasma (liquid portion of the blood) is too low, resulting in the organs not receiving enough oxygenated blood flow. The most common cause of postpartum hemorrhage is lack of effective contraction of the uterus after childbirth.[2]
- Pregnancy-related death (PRĔG-năn-sē ri-LĀ-tĭd dĕth): The Centers for Disease Control and Prevention defines a pregnancy-related death as the death of a woman during pregnancy or within one year of the end of pregnancy from a pregnancy complication, a chain of events initiated by pregnancy, or the aggravation of an unrelated condition by the physiologic effects of pregnancy. Most of these pregnancy-related deaths are preventable. It is important for all women of reproductive age to adopt healthy lifestyles (e.g., maintain a healthy diet and weight, be physically active, quit all substance use, prevent injuries) and address any health problems before getting pregnant. A healthy pregnancy begins before conception and continues with prenatal care, along with early recognition and management of complications if they arise.[3]
Congenital Anomaly
A congenital anomaly (kŏn-JĔN-ĭ-tăl ă-NOM-ă-lē) is an abnormality in a baby that is present at birth. Many congenital anomalies are caused by teratogens (tĕr-AT-ŏ-jĕnz), substances toxic to a developing fetus. For example, excessive alcohol intake by the mother can cause fetal alcohol spectrum disorder. Maternal diseases during pregnancy can also cause a birth defect or a chronic health problem. Some diseases that are known to potentially have an adverse effect on the fetus include diabetes, cytomegalovirus, toxoplasmosis, rubella, varicella, hypothyroidism, and infections caused by streptococcus B. For example, if an unvaccinated mother contracts rubella during the first three months of pregnancy, damage can occur to the baby’s eyes, ears, heart, or brain.[4]
Fetal Alcohol Spectrum Disorders
One of the most commonly used teratogens is alcohol. Because half of all pregnancies in the United States are unplanned, it is recommended that women of child-bearing age take great caution against drinking alcohol when not using birth control and when pregnant. Alcohol consumption, particularly during the second month of prenatal development, but at any point during pregnancy, may lead to neurocognitive and behavioral difficulties that can last a lifetime.[5]
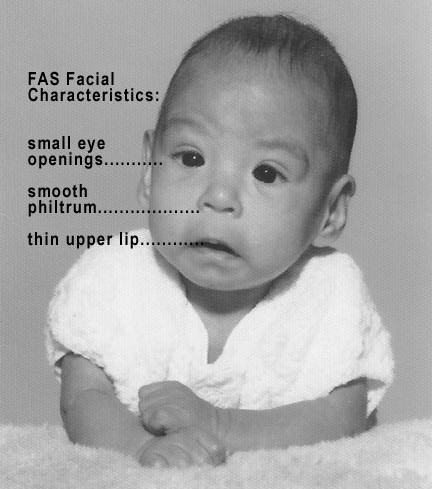
There is no acceptable safe limit for alcohol use during pregnancy, but binge drinking (five or more drinks on a single occasion) or having seven or more drinks during a single week places a child at particularly high risk. In extreme cases, alcohol consumption can lead to fetal death, but more frequently it can result in fetal alcohol spectrum disorders (FĒ-tăl AL-kŏ-hŏl SPEK-trŭm dĭs-ŎR-dĕrz) (FASD). This terminology is now used when looking at the effects of exposure and replaces the term fetal alcohol syndrome. It is preferred because it recognizes that symptoms occur on a spectrum and that all individuals do not have the same characteristics. Children with FASD share certain physical features such as flattened noses, small eye openings, small heads, intellectual developmental delays, and behavioral problems. See Figure 8.9[6] for an image of a child with FASD.[7]
Premature Labor and Premature Infant
Preterm labor (PRĒ-tûrm LĀ-bŏr) is defined as labor occurring between 20 and 37 weeks of gestation. There are many potential causes of preterm labor, such as stress, infection, placental abruption, placenta previa, substance use, history of preterm birth or abortion, inadequate prenatal care, smoking, maternal age <18 or >40, poor nutrition, low body mass index, fetal congenital anomaly, fetal growth restriction, oligohydramnios, polyhydramnios, vaginal bleeding, premature preterm rupture of membranes (prē-mă-CHŪR prē-tûrm RŬP-chĕr ŏv MEM-brānz) (PPROM), and other environmental factors.[8]
The main concern with premature labor is the prematurity of the infant, which can cause respiratory distress and impaired neurological development. A premature infant (prē-mă-CHŪR IN-fănt) refers to an infant who is born before completing 37 weeks of gestation. Treatment of premature labor is based on the gestational age at which the mother presents to the hospital and may include medications to stop labor from progressing, such as magnesium sulfate.[9]
Cerclage (sĕr-KLĂZH) is a procedure typically performed during the second semester of pregnancy to prevent preterm labor and miscarriage. During the procedure, the cervix is sewed shut with sutures to prevent dilation and premature delivery. It is performed in women whose cervix isn’t strong enough to stay closed as the pregnancy grows. The suture is removed when the fetus is full-term, which allows vaginal delivery to proceed. [10]
Miscarriage and Stillbirth
Pregnancy loss is experienced in over ten percent of pregnancies, typically due to chromosomal abnormalities before the 12th week of pregnancy. Miscarriage (MĬS-kăr-ĭj) refers to loss of a fetus before the 20th week of pregnancy. It typically causes cramping and bleeding, similar to heavy menses. In some cases, a surgical procedure called dilation and evacuation (D&E) is required. Normal menstrual cycles generally return within a few months.[11]
Stillbirth (STĬL-bûrth), also known as intrauterine fetal demise (ĬN-tră-YŪ-tə-rīn FĒT-ăl dĕ-MĪZ), refers to the loss of a fetus after 20 weeks’ gestation. About 24,000 babies are stillborn every year in the United States. Although many times the cause of the stillbirth is unknown, there are several potential causes, such as infection, chromosomal abnormalities, placental problems.[12]
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Wormer, Jamil, & Bryant and is licensed under CC BY 4.0 ↵
- Centers for Disease Control and Prevention. (2023, April 26). Preventing pregnancy-related deaths. Department of Health & Human Services. https://www.cdc.gov/reproductivehealth/maternal-mortality/preventing-pregnancy-related-deaths.html ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- “Photo_of_baby_with_FAS.jpg” by Teresa Kellerman is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Suman & Luther and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Suman & Luther and is licensed under CC BY 4.0 ↵
- The American College of Obstetricians and Gynecologists. (2021, November). Cervical cerclage. https://www.acog.org/womens-health/faqs/cervical-cerclage ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵
- This work is a derivative of Lifespan Development by Julie Lazzara and is licensed under CC BY 4.0 ↵

