Once dietary lipids are digested in the gastrointestinal tract and absorbed from the small intestine, they need to be transported around the body so they can be utilized by cells or stored for later use. Once again, the fact that lipids aren’t water-soluble means that they need some help getting around the watery environment of the body. Let’s take a look at how this works.
Lipoproteins Transport Lipids Around the Body
Lipoproteins are transport vehicles for moving water-insoluble lipids around the body. There are different types of lipoproteins that do different jobs. However, all are made up of the same four basic components: cholesterol, triglycerides, phospholipids, and proteins.
The interior of a lipoprotein—called the lipid core—carries the triglycerides and cholesterol esters, both of which are insoluble in water. Cholesterol esters are cholesterol molecules with a fatty acid attached. The exterior of lipoproteins—called the surface coat—is made up of components that are at least partially soluble in water: proteins (called apolipoproteins), phospholipids, and unesterified cholesterol. The phospholipids are oriented so that their water-soluble heads are pointed to the exterior, and their fat-soluble tails are pointed towards the interior of the lipoprotein. Apoliproteins are similarly amphipathic (soluble in both fat and water), a property that makes them useful for aiding in the transport of lipids in the blood.
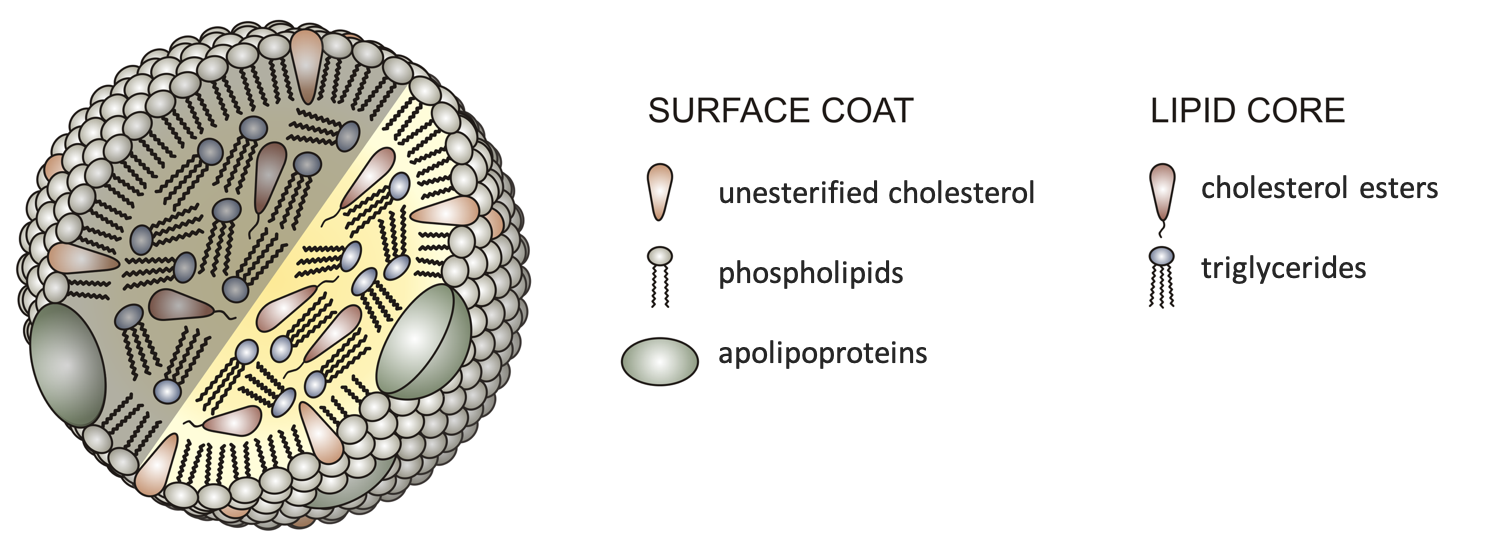
Figure 5.24. Basic structure of all lipoproteins. Note the orientation of phospholipids on the surface coat.
While all lipoproteins have this same basic structure and contain the same four components, different types of lipoproteins vary in the relative amounts of the four components, in their overall size, and in their functions. These are summarized in the graph and table below, and the following sections give more details on the role of each type of lipoprotein.
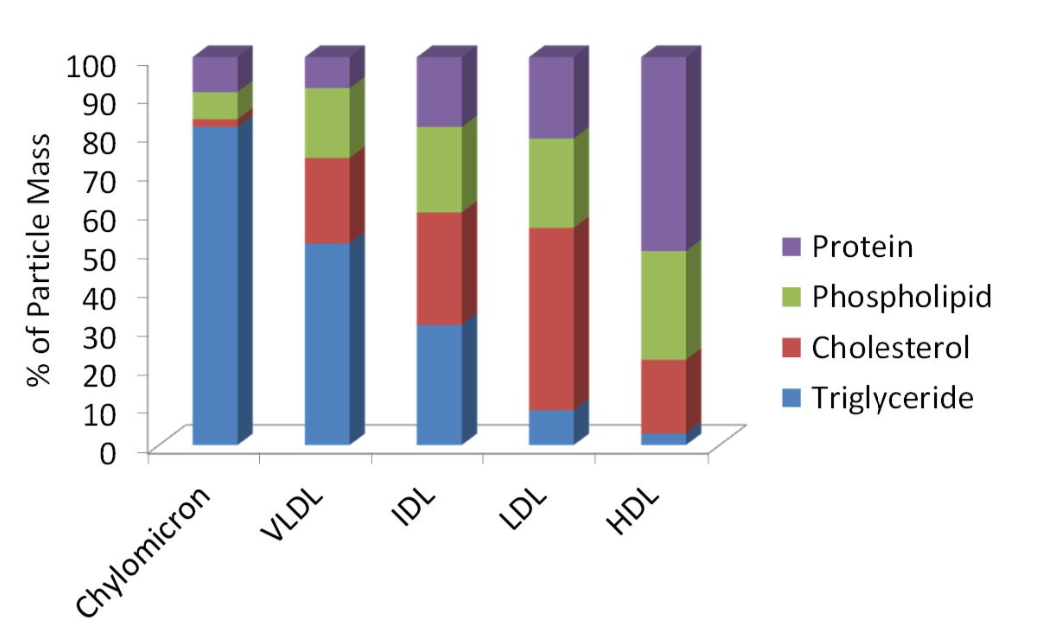
Figure 5.25. Comparison of composition of lipoproteins.
|
|
Chylomicrons |
Very-low-density lipoproteins (VLDL) |
Intermediate-density lipoproteins (IDL) |
Low-density lipoproteins (LDL) |
High-density lipoproteins (HDL) |
|
Diameter (nm) |
75-1200 (largest) |
30-80 |
25-35 |
18-25 |
5-12 (smallest) |
|
Density (g/dL) |
0.95 (least dense) |
0.95-1.006 |
1.006-1.019 |
1.019-1.063 |
1.063 (most dense) |
|
Function |
Transports lipids from the small intestine, delivers TG to the body’s cells |
Transports lipids from the liver, delivers TG to body’s cells |
Formed as VLDL become depleted in TG; either returned to liver or made into LDL |
Deliver cholesterol to cells |
Pick up cholesterol in the body and return to the liver for disposal |
Table 5.1. Comparison of composition, size, density, and function of lipoproteins. (TG = triglycerides)
Except for chylomicrons, the names of the lipoproteins refer to their density. Of the four components of lipoproteins, protein is the most dense and triglyceride is the least dense. (This is why one pound of muscle is much more compact in size than one pound of adipose or fat tissue.) High-density lipoproteins are the most dense of the lipoproteins, because they contain more protein and less triglyceride. Chylomicrons are the least dense, because they contain so much triglyceride and relatively little protein.
Chylomicrons Deliver Lipids to Cells for Utilization and Storage
On the previous page, we learned that chylomicrons are formed in the cells of the small intestine, absorbed into the lymph vessels, and then eventually delivered into the bloodstream. The job of chylomicrons is to deliver triglycerides (originating from digested food) to the cells of the body, where they can be used as an energy source or stored in adipose tissue for future use.
How do the triglycerides get from the chylomicrons into cells? An enzyme called lipoprotein lipase sits on the surface of cells that line the blood vessels. It breaks down triglycerides into fatty acids and glycerol, which can then enter nearby cells. If those cells need energy right away, they’ll oxidize the fatty acids to generate ATP. If they don’t need energy right away, they’ll reassemble the fatty acids and glycerol into triglycerides and store them for later use.
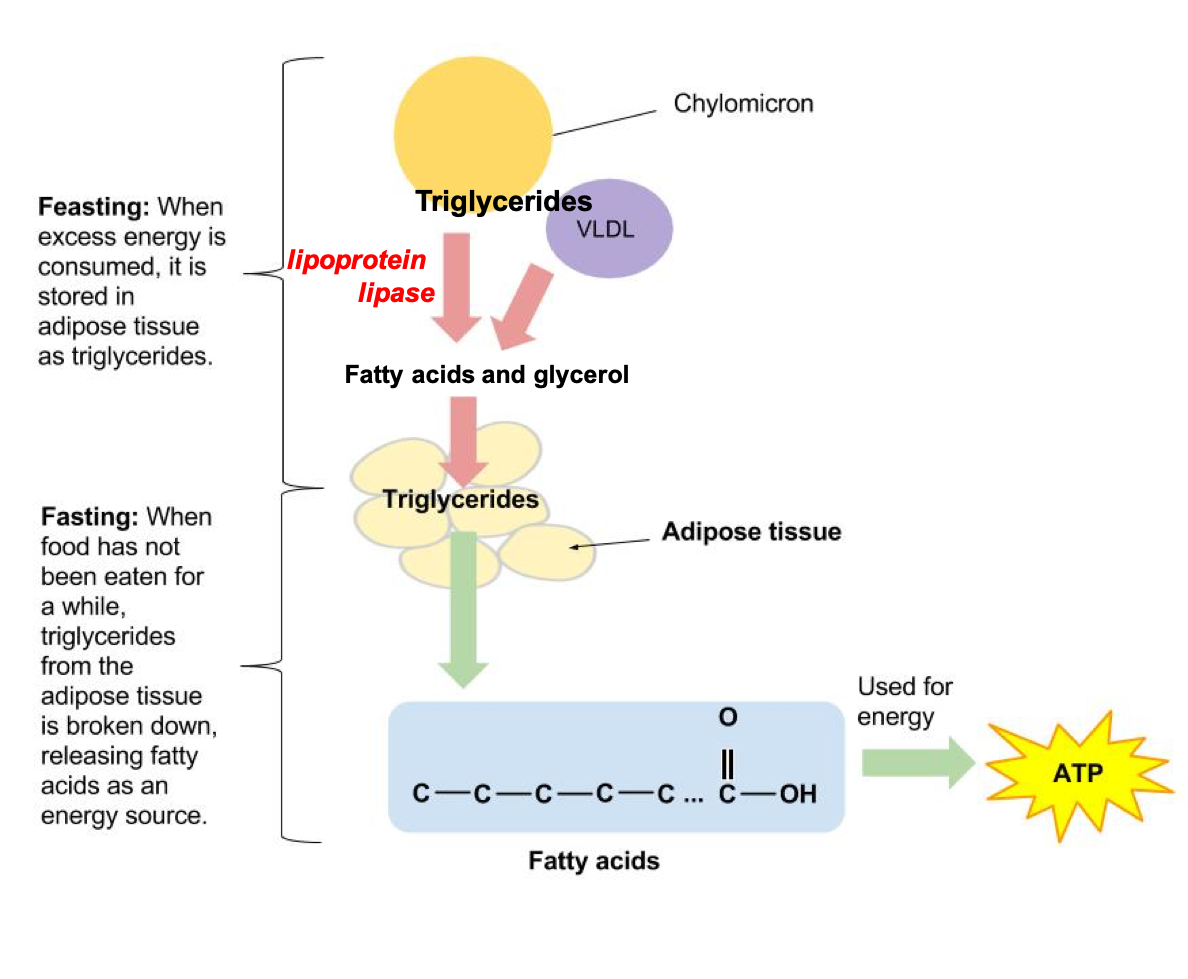
Figure 5.26. Triglycerides in chylomicrons and VLDL are broken down by lipoprotein lipase so that fatty acids and glycerol can be used for energy—or stored for later—in cells.
As triglycerides are removed from the chylomicrons, they become smaller. These chylomicron remnants travel to the liver, where they’re disassembled.
Lipid Transport from the Liver
The contents of chylomicron remnants, as well as other lipids in the liver, are incorporated into another type of lipoprotein called very-low-density lipoprotein (VLDL). Similar to chylomicrons, the main job of VLDL is delivering triglycerides to the body’s cells, and lipoprotein lipase again helps to break down the triglycerides so that they can enter cells (Figure 5.27).
As triglycerides are removed from VLDL, they get smaller and more dense, because they now contain relatively more protein compared to triglycerides. They become intermediate-density lipoproteins (IDL) and eventually low-density lipoproteins (LDL). The main job of LDL is to deliver cholesterol to the body’s cells. Cholesterol has many roles around the body, so this is an important job. However, too much LDL can increase a person’s risk of cardiovascular disease, as we’ll discuss below.
High-density lipoproteins (HDL) are made in the liver and gastrointestinal tract. They’re mostly made up of protein, so they’re very dense. Their job is to pick up cholesterol from the body’s cells and return it to the liver for disposal.
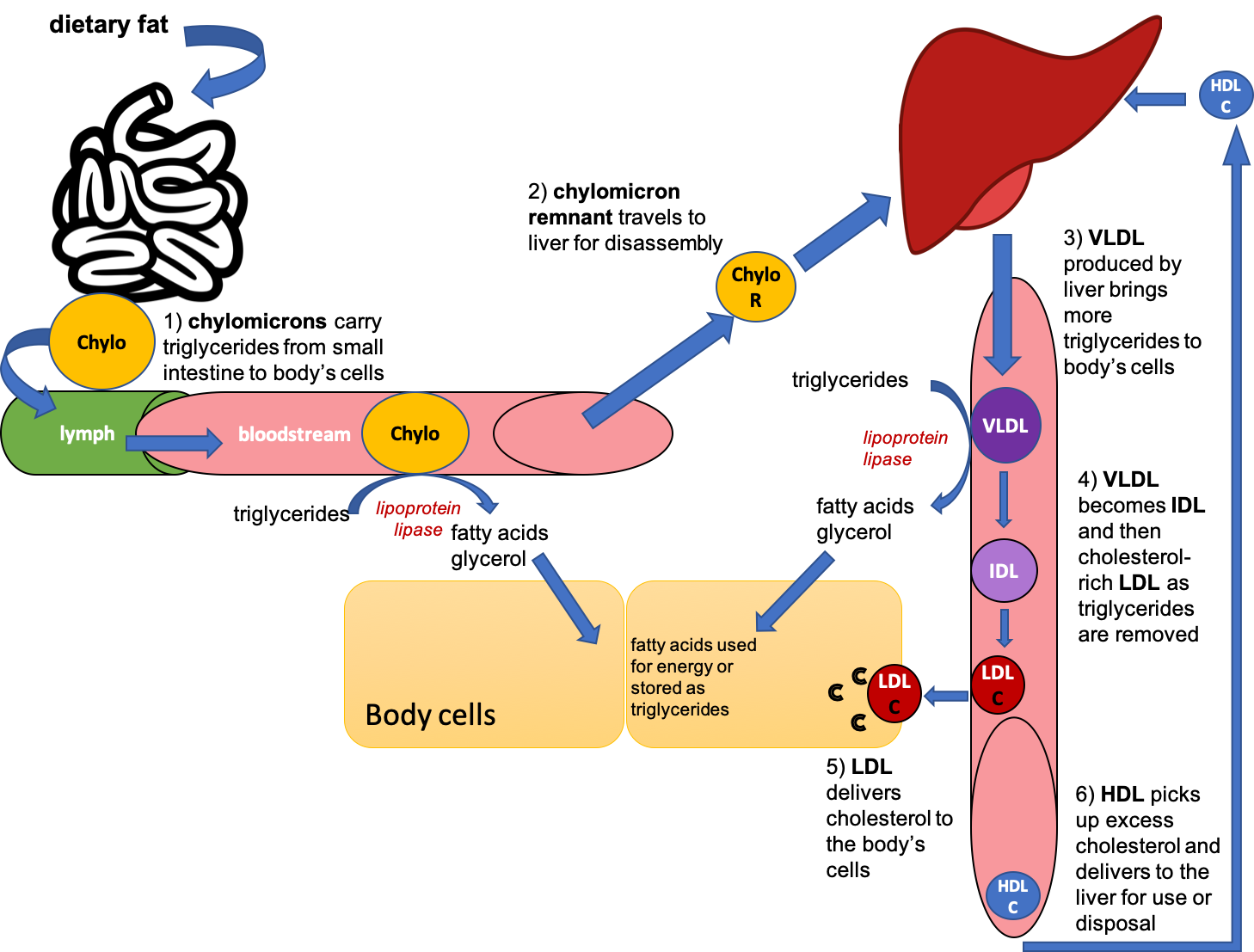
Figure 5.27. Overview of lipoprotein functions in the body.
VIDEO: “Cholesterol Metabolism, LDL, HDL, and Other Lipoproteins, Animation,” by Alila Medical Media, YouTube (May 1, 2018), 3:45 minutes.
Does Eating a Higher Fat Diet Mean You Will Store More Fat?
No. How much fat a person stores depends on how many calories they consume relative to how many calories they need to fuel their body. If they consume more calories than needed to meet their body’s daily needs—whether those calories come from dietary fat, carbohydrate, or protein—then they’ll store most of the excess calories in the form of fat in adipose tissue. If they consume a high-fat diet but not excess calories, then they’ll utilize that fat to generate ATP for energy. That said, remember that fat is more calorically dense (9 kilocalories per gram) than protein or carbohydrates (both 4 kcal/g), so if you eat a high-fat diet, you may need to eat smaller portions. And, as we’ll discuss later in this unit, there are good reasons to watch the type of fats that you eat, because of the relationship between dietary fat intake and risk of developing cardiovascular disease.
Understanding Blood Cholesterol Numbers
A person’s blood cholesterol numbers can be one indicator of their risk of developing cardiovascular disease. This is a standard blood test, also called a lipid panel, that reports total cholesterol, LDL, HDL, and triglycerides. When doctors assess a person’s risk of cardiovascular disease, they consider these numbers—along with other risk factors like family history, smoking, diabetes, and high blood pressure—in determining their recommendations for lifestyle changes (such as improving diet and getting more exercise) or prescribing medications.
You might be familiar with LDL and HDL as “bad cholesterol” and “good cholesterol,” respectively. This is an oversimplification to help people interpret their blood lipid values, because cholesterol is cholesterol; it’s not good or bad. The cholesterol in your food or synthesized in your body is all the same cholesterol molecule, and you can’t consume good or bad cholesterol. In reality, LDL and HDL are both lipoproteins that carry cholesterol. A more appropriate descriptor for LDL might be the “bad cholesterol transporter.” We can think of HDL as the “good cholesterol transporter,” although the more researchers learn about HDL, the more they realize that this is also an oversimplification.
What’s so bad about LDL? If there’s too much LDL in the blood, it can become lodged in arterial walls and contribute to the development of atherosclerosis, when fatty plaques thicken the walls of arteries and reduce the flow of blood (and therefore oxygen and nutrients). Atherosclerosis can lead to a number of problems, including the following:
- coronary artery disease (can lead to angina and heart attack)
- carotid artery disease (increases risk of stroke)
- peripheral artery disease
- chronic kidney disease
If a broken piece of plaque or a blood clot completely blocks an artery supplying the brain or the heart, it can cause a stroke or a heart attack, respectively. If you have high LDL cholesterol, then making changes like exercising more, eating less saturated fat, and stopping smoking (if applicable) can help lower it. Sometimes medications are also necessary to keep LDL in check.
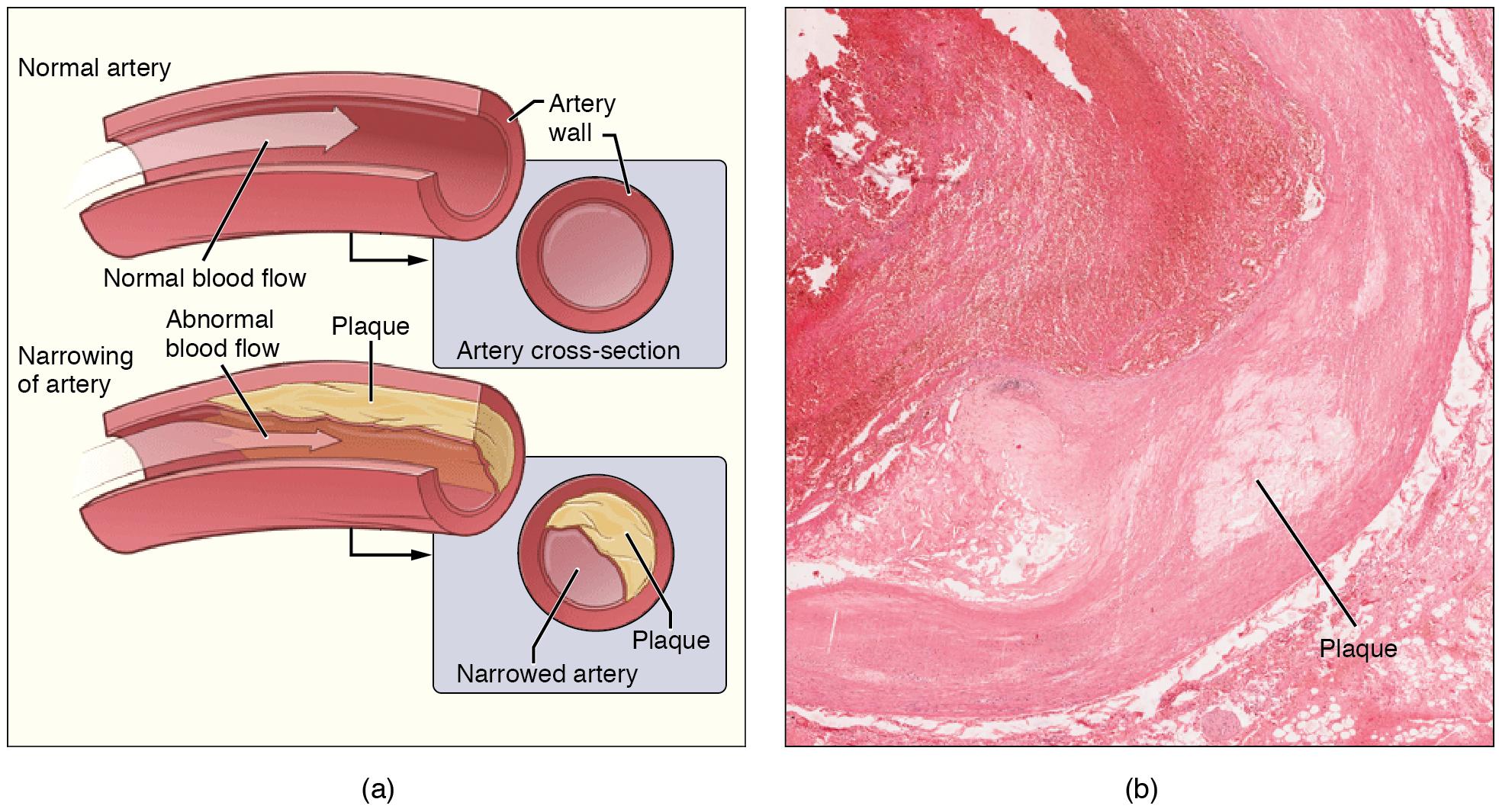
Fig. 5.28. Atherosclerosis. (a) Atherosclerosis can result from plaques formed by the buildup of fatty, calcified deposits in an artery. (b) Plaques can also take other forms, as shown in this micrograph of a coronary artery that has a buildup of connective tissue within the artery wall. LM × 40. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Physicians sometimes run additional blood tests to measure the LDL particle size and the number of LDL particles. The standard LDL test measures the total amount of cholesterol that is carried by LDL, but the reality is that LDL comes in a range of sizes, and small LDL particles are more strongly associated with the risk of atherosclerosis and cardiovascular disease than large LDL particles. For two people with the same total LDL cholesterol measurement, a person with more small particles will have a greater number of LDL particles circulating and a higher risk of developing heart disease. A person with more large LDL particles will have fewer particles overall and a lower risk of developing heart disease. Measuring particle size is not recommended for all patients because of the cost of the test and the fact that it rarely changes treatment course or improves outcomes. However, it can be useful in patients with diabetes or insulin resistance, as they tend to have more small LDL particles, which may call for using medications sooner or in higher doses.
HDL has been considered the “good cholesterol” or “good cholesterol transporter” because it scavenges cholesterol, including LDL lodged in the arterial walls, and helps to remove it from the body. Previously, it was thought that high HDL could prevent atherosclerosis and protect people from cardiovascular disease. But over the last few years, researchers have discovered that this view of HDL is oversimplified. Pharmaceutical companies developed drugs to raise HDL, thinking this would help to prevent cardiovascular disease. When these medications were tested in clinical trials, they were effective at raising HDL, but they didn’t decrease the incidence of heart attack, stroke, angina, or death from cardiovascular disease.1 In one clinical trial, the incidence of cardiovascular events and death from any cause were actually increased in people who took the HDL-raising medication (2). Genetic studies have also shown that people with genes for higher HDL don’t necessarily have a lower risk of developing cardiovascular disease.3 People with low HDL cholesterol do seem to have a higher risk of cardiovascular disease, but they also tend to have other risk factors like sedentary lifestyle, smoking, and diabetes. It’s not clear that low HDL is actually a cause of cardiovascular disease; we only know that it’s correlated. Because of these discoveries, raising HDL cholesterol is no longer considered a goal of prevention of heart disease. Rather, lowering LDL cholesterol is the primary target.4,5
Self-Check:
Attributions:
- Lindshield, B. L. Kansas State University Human Nutrition (FNDH 400) Flexbook. goo.gl/vOAnR, CC BY-NC-SA 4.0
- OpenStax, Anatomy and Physiology. OpenStax CNX. Aug 28, 2019 http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@16.7.
- University of Hawai‘i at Mānoa Food Science and Human Nutrition Program, “Digestion and Absorption of Lipids,” CC BY-NC 4.0
References:
- Rosenson, R. S. (2018). Measurement of blood lipids and lipoproteins—UpToDate. Retrieved October 7, 2019, from UpToDate website: https://www.uptodate.com/contents/measurement-of-blood-lipids-and-lipoproteins?search=lipid%20particle%20size&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
- Rosenson, R. S., & Durrington, P. (2017). HDL cholesterol: Clinical aspects of abnormal values—UpToDate. Retrieved October 7, 2019, from UpToDate website: https://www.uptodate.com/contents/hdl-cholesterol-clinical-aspects-of-abnormal-values?search=dyslipidemia%20guidelines&source=search_result&selectedTitle=7~150&usage_type=default&display_rank=7
- 1Lincoff, A. M. et al. Evacetrapib and Cardiovascular Outcomes in High-Risk Vascular Disease. New England Journal of Medicine 376, 1933–1942 (2017).
- 2 Barter, P. J. et al. Effects of Torcetrapib in Patients at High Risk for Coronary Events. New England Journal of Medicine 357, 2109–2122 (2007).
- 3Voight, B. F. et al. Plasma HDL cholesterol and risk of myocardial infarction: a mendelian randomisation study. Lancet 380, 572–580 (2012).
- 4Jacobson, T. A., Ito, M. K., Maki, K. C., Orringer, C. E., Bays, H. E., Jones, P. H., … Brown, W. V. (2015). National lipid association recommendations for patient-centered management of dyslipidemia: Part 1–full report. Journal of Clinical Lipidology, 9(2), 129–169. https://doi.org/10.1016/j.jacl.2015.02.003
- 5Catapano, A. L., Graham, I., De Backer, G., Wiklund, O., Chapman, M. J., Drexel, H., … Wald, D. (2016). 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. European Heart Journal, 37(39), 2999–3058. https://doi.org/10.1093/eurheartj/ehw272
Image Credits:
- Figure 5.24. “Structure of a Lipoprotein” by AntiSense is licensed under CC BY-SA 3.0
- Figure 5.25. Comparison of composition, size, density, and function of lipoproteins by Alice Callahan, CC BY 4.0, including Figure 4.712 from Lindshield, B. L. Kansas State University Human Nutrition (FNDH 400) Flexbook. goo.gl/vOAnR, CC BY-NC-SA 4.0
- Figure 5.26. “Storing and Using Fat” by Allison Calabrese is licensed under CC BY 4.0; with modifications by Alice Callahan.
- Figure 5.27. Overview of lipoprotein transport and delivery by Alice Callahan is licensed under CC BY 4.0; with liver by maritacovarrubias and small intestine by H Alberto Gongora, both from the Noun Project, CC BY 3.0
- Figure 5.28. “Atherosclerosis” by OpenStax is licensed under CC BY 4.0

