Now that we’ve covered the structures and functions of the digestive system, it should be clear that the digestion of food requires the coordinated action of multiple organs. If any of these aren’t working well, it can wreak havoc on the function of the entire system and interfere with health and quality of life. Let’s look at some common discomforts and disorders of the GI tract.
Heartburn and Gastroesophageal Reflux
Heartburn is a burning, often painful, sensation in the chest (behind the breastbone) or throat. Heartburn is caused by gastroesophageal reflux (GER), when the acidic chyme in the stomach escapes back into the esophagus and even into the mouth. Normally, this reflux is prevented by the lower esophageal sphincter (a tight ring of muscle) that sits between the esophagus and stomach. The muscles of the sphincter contract to keep it closed, only relaxing to allow food boluses and liquid to pass from the esophagus into the stomach and then quickly contracting again to keep the contents of the stomach separate from the esophagus. The lower esophageal sphincter can be weakened because of increased pressure on the abdomen from obesity or pregnancy, exposure to tobacco smoke, and some medications, so the risk of GER is increased in these scenarios.
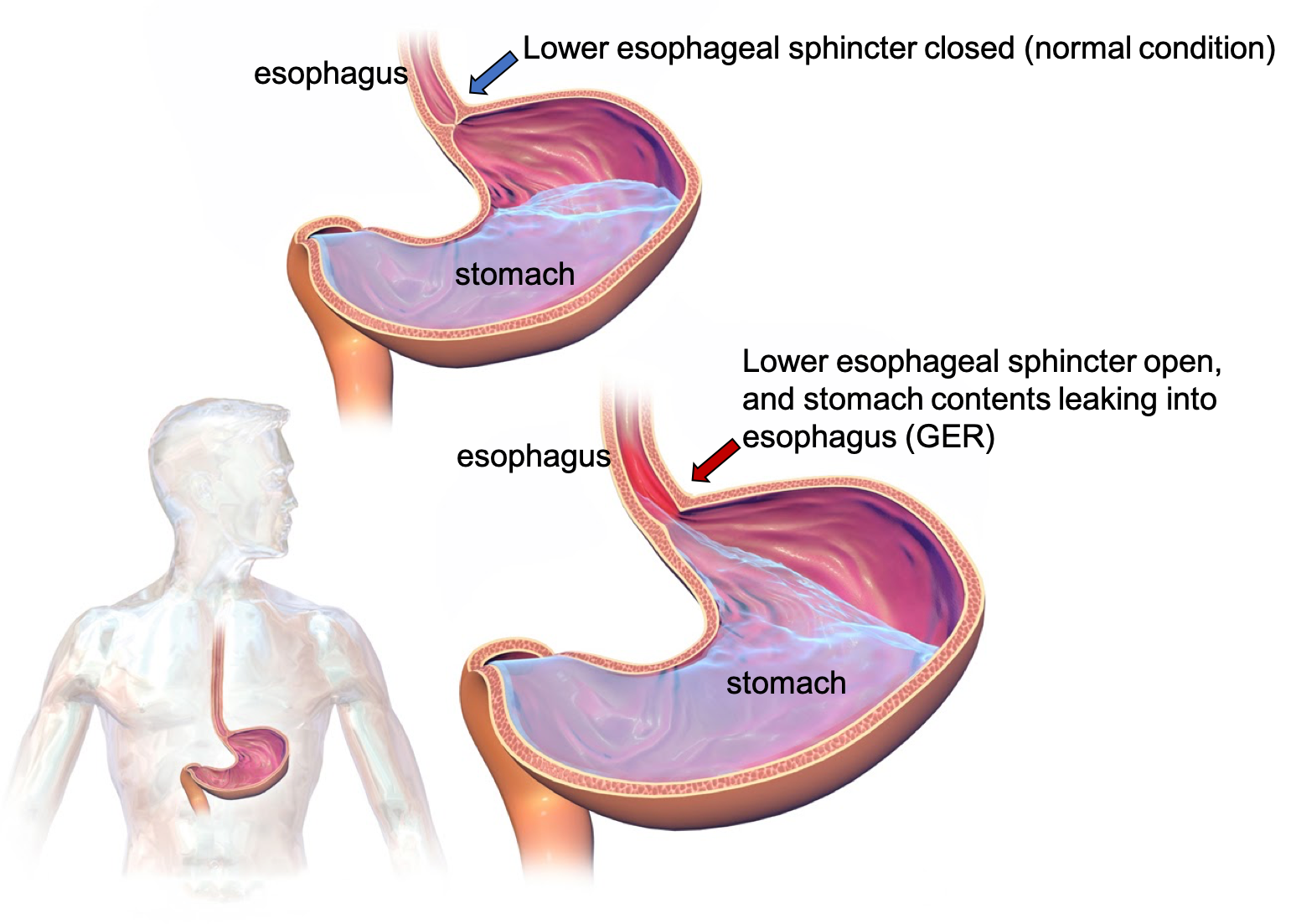
Figure 3.15. In gastroesophageal reflux, the acidic contents of the stomach escape backwards into the esophagus, causing pain and burning sensations in the chest and/or throat.
Occasional heartburn is a common complaint, especially after eating large greasy or spicy meals. However, if it occurs more than twice per week, it may be diagnosed as gastroesophageal reflux disease (GERD), which should be treated not only to relieve the discomfort that it causes but also to prevent damage to the tissues of the esophagus, which can increase the risk of cancer. In addition to heartburn, GER and GERD can cause difficult and painful swallowing, a persistent sore throat or cough, a sense that there’s a lump in your throat, and nausea and vomiting.
The symptoms of GER and GERD can often be addressed through diet and lifestyle changes, including the following:
- Avoid foods that seem to trigger symptoms. Common culprits are greasy or spicy foods, chocolate, coffee, peppermint, alcohol, and acidic foods such as tomatoes or citrus.
- Eat smaller, more frequent meals instead of large meals.
- Avoid eating 3 hours before bedtime, and stay upright for 3 hours after eating.
- Wear clothing that is loose around the abdomen.
- Raise the head of your bed by 6 to 8 inches by placing blocks under the bedposts. (Extra pillows will not help.)
- Quit smoking and avoid secondhand smoke, if needed.
- Lose weight, if needed.
Over-the-counter medications like antacids (Maalox, Mylanta, Rolaids) can also help with occasional heartburn. If symptoms are persistent and frequent, it’s wise to see a doctor to be checked out for GERD and to discuss other treatment and medication options.1,2
Peptic Ulcers
Peptic ulcers are sores on the tissues lining the esophagus, stomach, or duodenum (the first section of the small intestine). They occur when the mucous coating the GI tissues is damaged, exposing the tissue to pepsin and hydrochloric acid. This further erodes away the tissues, causing pain if it damages a nerve and bleeding if it damages a blood vessel. Ulcers are most serious if they perforate the wall of the GI tract, which can cause a serious infection. Peptic ulcers cause stomach pain, often when the stomach is empty, and may go away when you eat or take antacids. In the most serious cases, blood may be seen in vomit and/or the stool, and the patient may have very sharp and persistent stomach pain.
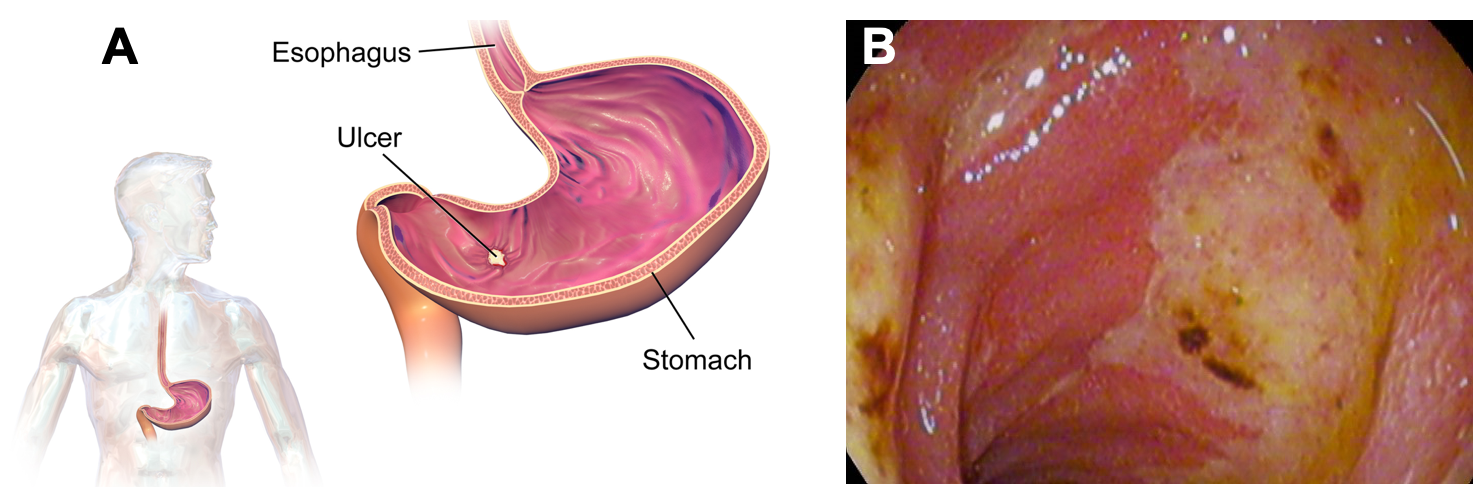
Figure 3.16. Peptic ulcers. (A) The location of a peptic ulcer in the stomach. (B) A photo from an endoscopy of a patient with an ulcer in the duodenum.
Doctors used to believe that stress and excessive stomach acid caused peptic ulcers, so they would recommend a bland diet, stress reduction, and acid-suppressing medications as treatment. However, these treatments often didn’t work, because they weren’t actually treating the root cause of the ulcers. We now know that there are two main causes of peptic ulcers. The first and most common cause is infection with a bacteria called Helicobacter pylori (H. pylori). H. pylori infection is very common, with about 50% of the population worldwide harboring the bacteria, most of them living without any symptoms. It’s not certain how people are infected with H. pylori or why they cause ulcers in some people and not in others. However, understanding the link between H. pylori and ulcers was an important discovery, because it led to effective treatments. The H. pylori bacteria are able to survive the acidic environment of the stomach, and they damage the mucous coating of the GI tract, leaving it vulnerable to further damage from acid and pepsin. Ulcers caused by H. pylori infection are treated with antibiotics to kill the bacteria, with the addition of an acid-suppressing medication to allow the tissue to heal.
The second major cause of peptic ulcers is long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen. One of the side effects of NSAIDS is that they block the production of an enzyme that protects the stomach lining, so using these medications frequently and chronically can increase the risk of developing a stomach ulcer. To treat an ulcer caused by NSAIDs, doctors recommend stopping or reducing the use of NSAIDs. They may also prescribe an acid-reducing medication to allow the tissue to heal.3
Diarrhea and Constipation
Both diarrhea and constipation can occur if the normal function and rhythm of the GI tract is disrupted. If waste matter moves too quickly through the large intestine, not enough water is absorbed, resulting in the loose, watery stools characteristic of diarrhea. This is most commonly caused by ingesting food or water contaminated with bacteria (e.g., E. coli, Salmonella), viruses (e.g., norovirus, rotavirus), or parasites (e.g., Cryptosporidium enteritis, Giardia lamblia). Dietary allergies and intolerances can also cause diarrhea, as we’ll discuss on the next page. Complications of diarrhea include dehydration and malabsorption of nutrients.4
On the other end of the spectrum is constipation, characterized by infrequent bowel movements (less than 3 times per week) with stools that are hard, dry, or lumpy, and often painful to pass. Sometimes, constipation is caused by holding stool and delaying defecation. That gives the colon and rectum additional time to absorb water, making the feces too hard and dry. Delaying defecation is common in children or others who may fear that it will hurt to pass a stool, but of course, holding it only worsens the problem. Constipation can also occur due to other disruptions in daily rhythms, such as changing what or how much you eat, travel, or medication changes. Constipation is common in pregnancy due to hormonal changes. It also becomes more common with age, which may be due to decreased physical activity, medication use, or weakness in the smooth muscle of the intestine. Constipation can be a sign of another medical problem, so chronic constipation should be checked out by a doctor.
Constipation can often be addressed by dietary changes, including eating more high-fiber foods (whole grains, legumes, fruits, vegetables, nuts, etc.) and drinking more water. It can also be helpful to attempt a bowel movement after meals, when the intestine is more active, and to make that a habit to try to establish more regularity in bowel movements. A caffeinated beverage with breakfast can help, as can increasing physical activity.
Fiber supplements such as Metamucil, Citrucel, or Benefiber can be helpful for increasing fiber intake and addressing constipation, at least in the short term. However, it’s preferable to transition to dietary sources of fiber, as they come packaged with many other valuable nutrients.
Laxatives may also be helpful to address constipation in the short-term but are usually not a good long-term solution. It’s possible to become dependent on some types of laxatives for bowel movements, meaning that the colon doesn’t contract normally on its own. In these cases, a doctor can help make a plan to gradually reduce laxative use and find other ways to improve bowel regularity.4

Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (IBS) is a type of functional GI disorder, meaning that it’s caused by a disruption in the signals between the brain and gut. People suffering from IBS often experience abdominal pain, bloating, the feeling that they can’t finish a bowel movement, as well as diarrhea or constipation or both, often in cycles. IBS is common; about 12% of people in the U.S. are thought to have it. It’s more common in women, seems to run in families, and is often associated with stress, history of trauma, or severe GI infections. IBS isn’t well understood. It’s not clear what causes it, and it may have different causes in different people.5
Of course, since the cause of IBS isn’t understood, that lack of understanding makes it difficult to treat. Some people find that eating more fiber-rich foods and increasing physical activity improve their symptoms, so these are good first steps (and good for health regardless of their effect on IBS). Others find that following a diet that is low in carbohydrates called FODMAPs helps their symptoms. FODMAPs are fermentable carbohydrates found in many foods and can usually be eaten without issue by most people. Foods that are high in FODMAPs include fruits, vegetables, legumes, dairy products, wheat, and honey, so this is a very restrictive diet and should only be attempted with the guidance of a dietitian. Without careful planning, a low-FODMAP diet can be deficient in fiber, vitamins, and minerals. It is usually followed for just a few weeks, and if it helps with symptoms, foods are gradually added back to see what can be tolerated.6,7
In addition to dietary strategies, physicians sometimes prescribe medications to treat the symptoms of diarrhea or constipation associated with IBS.8
Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease (IBD) includes two types of disorders: ulcerative colitis and Crohn’s disease. Ulcerative colitis is specific to the large intestine (colon) and rectum, whereas Crohn’s disease can affect any part of the GI tract. Both are chronic inflammatory conditions in which symptoms may periodically flare and become more severe. IBD is often confused with IBS, because of the similarities in their names and some symptoms. However, they are different disorders with different causes. IBD is generally more severe and long-lasting, and it causes damage to the GI tract that can be seen on endoscopy (when a camera is inserted into the GI tract to visualize the interior). It’s important to get an accurate diagnosis of IBD in order to treat the disorder appropriately.9
Common symptoms of IBD are diarrhea, cramping and abdominal pain, feeling tired, and weight loss. IBD may be caused by autoimmune reactions (in which the immune system attacks the body’s own cells, in this case the cells of the GI tract) or certain genes, and other causes are being investigated. IBD often develops in people during adolescence or in their 20s. It may be treated with medications to reduce inflammation or modulate the immune system, or sometimes surgery.10,11
Self-Check:
References
- 1Kahrilas, P. J. (2019, October 24). Patient education: Gastroesophageal reflux disease in adults (Beyond the Basics)—UpToDate. UpToDate. https://www.uptodate.com/contents/gastroesophageal-reflux-disease-in-adults-beyond-the-basics?search=GER&topicRef=2265&source=see_link
- 2National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Acid Reflux (GER & GERD) in Adults. National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved February 23, 2020, from https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults
- 3National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Peptic Ulcers (Stomach Ulcers). National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved February 23, 2020, from https://www.niddk.nih.gov/health-information/digestive-diseases/peptic-ulcers-stomach-ulcers
- 4National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Constipation. National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved February 23, 2020, from https://www.niddk.nih.gov/health-information/digestive-diseases/constipation
- 5National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Irritable Bowel Syndrome (IBS). National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved February 23, 2020, from https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome
- 6Harvard Health Publishing. Try a FODMAPs diet to manage irritable bowel syndrome. Harvard Health. Retrieved February 23, 2020, from https://www.health.harvard.edu/diet-and-weight-loss/a-new-diet-to-manage-irritable-bowel-syndrome
- 7Slomski, A. (2020). The Low-FODMAP Diet Helps IBS Symptoms, but Questions Remain. JAMA. https://doi.org/10.1001/jama.2020.0691
- 8Wald, A. (2019, October 23). Treatment of irritable bowel syndrome in adults—UpToDate. UpToDate. https://www.uptodate.com/contents/treatment-of-irritable-bowel-syndrome-in-adults?search=IBS&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H2957204
- 9Crohn’s and Colitis Foundation. IBS vs IBD. Crohn’s & Colitis Foundation. Retrieved February 23, 2020, from https://www.crohnscolitisfoundation.org/what-is-ibd/ibs-vs-ibd
- 10National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (n.d.-a). Crohn’s Disease. National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved February 23, 2020, from https://www.niddk.nih.gov/health-information/digestive-diseases/crohns-disease
- 11National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Ulcerative Colitis. National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved February 23, 2020, from https://www.niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis
Images:
- Figure 3.15. “GastroEsophageal Reflux Disease” by BruceBlaus is licensed under CC BY-SA 4.0
- Figure 3.16. (a) “Gastric ulcer” by BruceBlaus is licensed under CC BY-SA 4.0 ; (b) “Duodenal ulcer A2 stage, acute duodenal mucosal lesion(ADML)” by melvil is licensed under CC BY-SA 4.0
- “Abdominal pain” by derneuemann is in the Public Domain, CC0

