5.4-Mechanisms of Antibacterial Drugs
0.2 Mechanisms of Antibacterial Drugs
Learning Objective
- Describe the mechanisms of action associated with drugs that inhibit cell wall biosynthesis, protein synthesis, membrane function, nucleic acid synthesis, and metabolic pathways
An important quality for an antimicrobial drug is selective toxicity, meaning that it selectively kills or inhibits the growth of microbial targets while causing minimal or no harm to the host. Most antimicrobial drugs currently in clinical use are antibacterial because the prokaryotic cell provides a greater variety of unique targets for selective toxicity, in comparison to fungi, parasites, and viruses. Each class of antibacterial drugs has a unique mode of action (the way in which a drug affects microbes at the cellular level), and these are summarized in Figure 10.4 and Table 10.1.
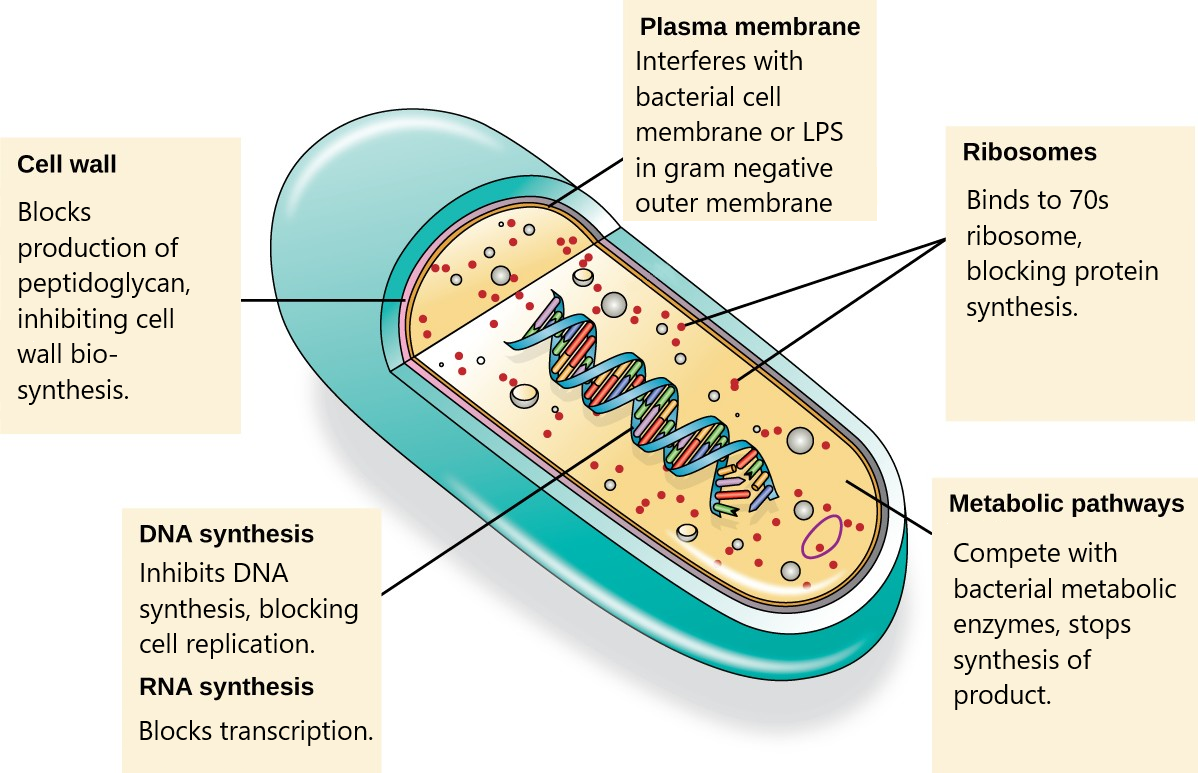
|
Mode of Action |
Target |
Drug Class |
|
Inhibit cell wall biosynthesis |
Penicillin-binding proteins |
β-lactams: penicillins, cephalosporins, monobactams, carbapenems |
|
Peptidoglycan subunits |
Glycopeptides |
|
|
Peptidoglycan subunit transport |
Bacitracin |
|
|
Inhibit biosynthesis of proteins |
30S ribosomal subunit |
Aminoglycosides, tetracyclines |
|
50S ribosomal subunit |
Macrolides, lincosamides, chloramphenicol, oxazolidinones |
|
|
Disrupt membranes |
Lipopolysaccharide, inner and outer membranes |
Polymyxin B, colistin, daptomycin |
|
Inhibit nucleic acid synthesis |
RNA |
Rifamycin |
|
DNA |
Fluoroquinolones |
|
|
Antimetabolites |
Folic acid synthesis enzyme |
Sulfonamides, trimethoprim |
|
Mycolic acid synthesis enzyme |
Isonicotinic acid hydrazide |
|
|
Mycobacterial adenosine triphosphate (ATP) synthase inhibitor |
Mycobacterial ATP synthase |
Diarylquinoline |
Table 10.1
Inhibitors of Cell Wall Biosynthesis
Several different classes of antibacterials block steps in the biosynthesis of peptidoglycan, making cells more susceptible to osmotic lysis (Table 10.2). Therefore, antibacterials that target cell wall biosynthesis are bactericidal in their action. Because human cells do not make peptidoglycan, this mode of action is an excellent example of selective toxicity. Antibiotics that inhibit the cell wall biosynthesis of bacteria include the penicillins (including ampicillin, amoxicillin, and methicillin), cephalosporins, vancomycin, and bacitracin. Although it may be administered orally or intramuscularly in some circumstances, bacitracin has been shown to be nephrotoxic (damaging to the kidneys). Therefore, it is more commonly combined with neomycin and polymyxin in topical ointments such as Neosporin.
Some of these antibiotics are natural antibiotics produced by fungi or bacteria, while others are semi-synthetic, where a natural antibiotic has been chemically modified in the lab.
|
Mechanism of Action |
Drug Class |
Specific Drugs |
Natural or Semisynthetic |
Spectrum of Activity |
|
Interact directly with PBPs and inhibit transpeptidase activity |
Penicillins |
Penicillin G, penicillin V |
Natural |
Narrow-spectrum against gram-positive and a few gram-negative bacteria |
|
|
|
Ampicillin, amoxicillin |
Semisynthetic |
Narrow-spectrum against gram-positive bacteria but with increased gram- negative spectrum |
|
Methicillin |
Semisynthetic |
Narrow-spectrum against gram-positive bacteria only, including strains producing penicillinase |
Table 10.2
|
Mechanism of Action |
Drug Class |
Specific Drugs |
Natural or Semisynthetic |
Spectrum of Activity |
|
|
Cephalosporins |
Cephalosporin C |
Natural |
Narrow-spectrum similar to penicillin but with increased gram-negative spectrum |
|
First- generation cephalosporins |
Semisynthetic |
Narrow-spectrum similar to cephalosporin C |
||
|
Second- generation cephalosporins |
Semisynthetic |
Narrow-spectrum but with increased gram-negative spectrum compared with first generation |
||
|
Third- and fourth- generation cephalosporins |
Semisynthetic |
Broad-spectrum against gram-positive and gram- negative bacteria, including some β- lactamase producers |
||
|
Fifth- generation cephalosporins |
Semisynthetic |
Broad-spectrum against gram-positive and gram- negative bacteria, including MRSA |
||
|
Monobactams |
Aztreonam |
Semisynthetic |
Narrow-spectrum against gram-negative bacteria, including some β- lactamase producers |
|
|
Carbapenems |
Imipenem, meropenem, doripenem |
Semisynthetic |
Broadest spectrum of the β-lactams against gram- positive and gram- negative bacteria, including many β- lactamase producers |
|
|
Large molecules that bind to the peptide chain of peptidoglycan subunits, blocking transglycosylation and transpeptidation |
Glycopeptides |
Vancomycin |
Natural |
Narrow spectrum against gram-positive bacteria only, including multidrug- resistant strains |
|
Block transport of |
Bacitracin |
Bacitracin |
Natural |
Broad-spectrum against |
|
peptidoglycan subunits |
|
|
|
gram-positive and gram- |
|
across cytoplasmic |
|
|
|
negative bacteria |
|
membrane |
|
|
|
|
Table 10.2
- Describe the mode of action of β-lactams.
Inhibitors of Protein Biosynthesis
The cytoplasmic ribosomes found in animal cells (80S) are structurally distinct from those found in bacterial cells (70S), making protein biosynthesis a good selective target for antibacterial drugs. Several types of protein biosynthesis inhibitors are discussed in this section and are summarized in Figure 10.5 and Table 10.3.
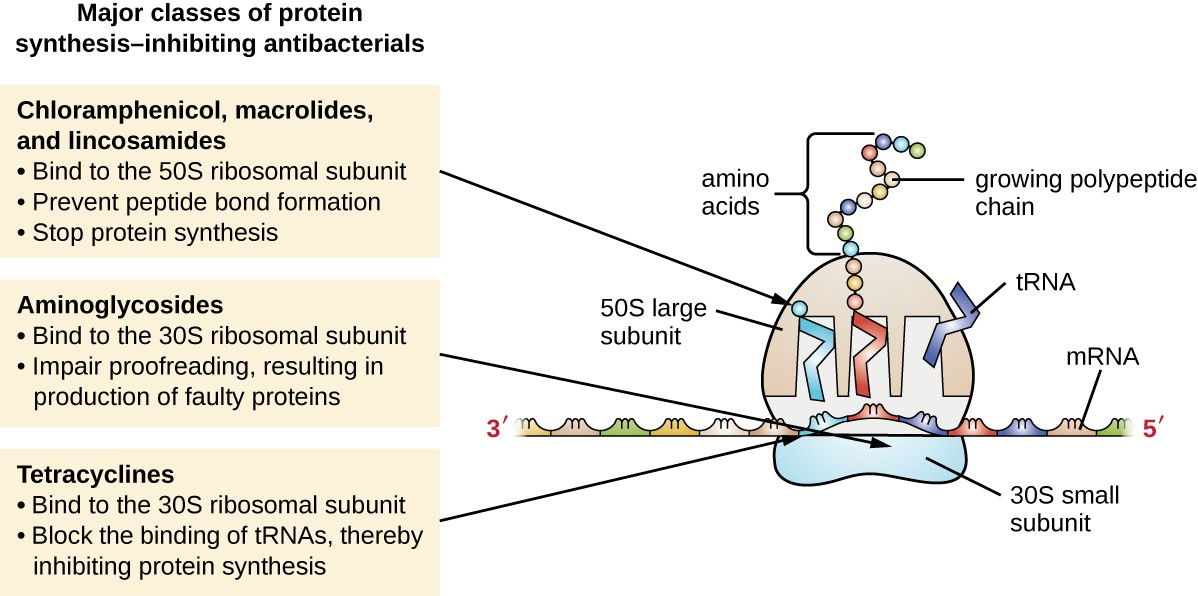
Protein Synthesis Inhibitors That Bind the 30S Subunit
Aminoglycosides are large, highly polar antibacterial drugs that bind to the 30S subunit of bacterial ribosomes, impairing the proofreading ability of the ribosomal complex responsible for making cellular proteins. The aminoglycosides, which include drugs such as streptomycin, gentamicin, neomycin, and kanamycin, are potent broad-spectrum antibacterials. However, aminoglycosides have been shown to be nephrotoxic (damaging to kidney), neurotoxic (damaging to the nervous system), and ototoxic (damaging to the ear).
Another class of antibacterial compounds that bind to the 30S subunit is the tetracyclines. In contrast to aminoglycosides, these drugs are bacteriostatic and inhibit protein synthesis by blocking the association of tRNAs with the ribosome during translation. Although the tetracyclines are broad spectrum in their coverage of bacterial pathogens, side effects that can limit their use include phototoxicity, permanent discoloration of developing teeth, and liver toxicity with high doses or in patients with kidney impairment.
Protein Synthesis Inhibitors That Bind the 50S Subunit
There are several classes of antibacterial drugs that work through binding to the 50S subunit of bacterial ribosomes. Specific examples include erythromycin, azithromycin, and chloramphenicol. The first drug discovered in this category was erythromycin. It was isolated in 1952 from Streptomyces erythreus. Compared with erythromycin, azithromycin has a broader spectrum of activity, fewer side effects, and a significantly longer half-life (1.5 hours for erythromycin versus 68 hours for azithromycin) that allows for once-daily dosing and a short 3-day course of therapy (i.e., Zpac formulation) for most infections.
The drug chloramphenicol represents yet another structurally distinct class of antibacterials that also bind to the 50S ribosome, inhibiting peptide bond formation. Chloramphenicol, produced by Streptomyces venezuelae, was discovered in 1947; in 1949, it became the first broad-spectrum antibiotic that was approved by the FDA. Although it is a natural antibiotic, it is also easily synthesized and was the first antibacterial drug synthetically mass produced. As a result of its mass production, broad-spectrum coverage, and ability to penetrate into tissues efficiently, chloramphenicol was historically used to treat a wide range of infections, from meningitis to typhoid fever to conjunctivitis. Unfortunately, serious side effects, such as lethal gray baby syndrome, and suppression of bone marrow production, have limited its clinical role. Because of toxicity concerns, chloramphenicol usage in humans is now rare in the United States and is limited to severe infections unable to be treated by less toxic antibiotics. Because its side effects are much less severe in animals, it is used in veterinary medicine.
|
Molecular Target |
Mechanism of Action |
Drug Class |
Specific Drugs |
Bacteriostatic or Bactericidal |
Spectrum of Activity |
|
30S subunit |
Causes mismatches between codons and anticodons, leading to faulty proteins that insert into and disrupt cytoplasmic membrane |
Aminoglycosides |
Streptomycin, gentamicin, neomycin, kanamycin |
Bactericidal |
Broad spectrum |
|
Blocks association of tRNAs with ribosome |
Tetracyclines |
Tetracycline, doxycycline, tigecycline |
Bacteriostatic |
Broad spectrum |
|
|
50S subunit |
Blocks peptide bond formation between amino acids |
Macrolides |
Erythromycin, azithromycin, telithromycin |
Bacteriostatic |
Broad spectrum |
|
Lincosamides |
Lincomycin, clindamycin |
Bacteriostatic |
Narrow spectrum |
||
|
Not applicable |
Chloramphenicol |
Bacteriostatic |
Broad spectrum |
||
|
Interferes with the formation of the initiation complex between 50S and 30S subunits and other factors. |
Oxazolidinones |
Linezolid |
Bacteriostatic |
Broad spectrum |
Table 10.3
![]()
- Compare and contrast the different types of protein synthesis inhibitors.
Inhibitors of Membrane Function
A small group of antibacterials target the bacterial membrane as their mode of action (Table 10.4). The polymyxins are natural polypeptide antibiotics that were first discovered in 1947 as products of Bacillus polymyxa; only polymyxin B and polymyxin E (colistin) have been used clinically. They are lipophilic with detergent-like properties and interact with the lipopolysaccharide component of the outer membrane of gram-negative bacteria, ultimately disrupting both their outer and inner membranes and killing the bacterial cells. Unfortunately, the membrane-targeting mechanism is not a selective toxicity, and these drugs also target and damage the membrane of cells in the kidney and nervous system when administered systemically. Because of these serious side effects and their poor absorption from the digestive tract, polymyxin B is used in over-the-counter topical antibiotic ointments (e.g., Neosporin), and oral colistin was historically used only for bowel decontamination to prevent infections originating from bowel microbes in immunocompromised patients or for those undergoing certain abdominal surgeries. The antibacterial daptomycin is a cyclic lipopeptide produced by Streptomyces roseosporus that seems to work like the polymyxins, inserting in the bacterial cell membrane and disrupting it. However, in contrast to polymyxin B and colistin, which target only gram-negative bacteria, daptomycin specifically targets gram-positive bacteria. It is typically administered intravenously and seems to be well tolerated, showing reversible toxicity in skeletal muscles.
|
Mechanism of Action |
Drug Class |
Specific Drugs |
Spectrum of Activity |
Clinical Use |
|
Interacts with lipopolysaccharide in the outer membrane of gram-negative bacteria, killing the cell through the eventual disruption of the outer membrane and cytoplasmic membrane
|
Polymyxins |
Polymyxin B |
Narrow spectrum against gram-negative bacteria, including multidrug-resistant strains |
Topical preparations to prevent infections in wounds
|
|
|
||||
|
|
|
|||
|
|
|
|||
|
|
|
|||
|
|
|
|||
|
|
|
|||
|
|
|
|||
|
|
|
|||
|
|
Polymyxin E (colistin)
|
Narrow spectrum against gram-negative bacteria, including multidrug-resistant strains
|
Oral dosing to decontaminate bowels to prevent infections in immunocompromised patients or patients undergoing invasive surgery/procedures.
|
|
|
|
||||
|
|
||||
|
|
||||
|
|
||||
|
|
||||
|
|
||||
|
|
||||
|
Intravenous dosing to treat serious systemic infections caused by multidrug-resistant pathogens |
||||
|
|
||||
|
|
||||
|
|
||||
|
|
|
|||
|
Inserts into the cytoplasmic membrane of gram-positive bacteria, disrupting the membrane and killing the cell
|
Lipopeptide |
Daptomycin |
Narrow spectrum against gram-positive bacteria, including
|
Complicated skin and skin-structure infections and bacteremia caused by gram-positive pathogens, including MRSA
|
|
|
|
|||
|
|
|
|||
|
|
|
|||
|
|
|
|||
|
|
|
|||
|
|
|
Table 10.4
![]()
- How do polymyxins inhibit membrane function?
Inhibitors of Nucleic Acid Synthesis
Some antibacterial drugs work by inhibiting nucleic acid synthesis (Table 10.5). The drug rifampin is a semisynthetic member of the rifamycin family and functions by blocking RNA polymerase activity in bacteria. The RNA polymerase enzymes in bacteria are structurally different from those in eukaryotes, providing for selective toxicity against bacterial cells. It is used for the treatment of a variety of infections, but its primary use, often in a cocktail with other antibacterial drugs, is against mycobacteria that cause tuberculosis. Despite the selectivity of its mechanism, rifampin can induce liver enzymes to increase metabolism of other drugs being administered (antagonism), leading to hepatotoxicity (liver toxicity) and negatively influencing the bioavailability and therapeutic effect of the companion drugs.
Fluoroquinolones, such as ciprofloxacin, kills bacterial cells by blocking DNA replication.
| Mechanisms of Action | Drug Class | Specific Drugs | Spectrum of activity | Clinical Use |
| Inhibits bacterial RNA polymerase activity and blocks transcription, killing the cell | Rifamycin | Rifampin | Narrow spectrum with activity against gram-positive and limited numbers of gram-negative bacteria. Also active against Mycobacterium tuberculosis. | Combination therapy for treatment of tuberculosis |
| Inhibits the activity of DNA gyrase and blocks DNA replication, killing the cell | Fluoroquinolones | Ciprofloxacin, ofloxacin, moxifloxacin | Broad spectrum against gram-positive and gram-negative bacteria | Wide variety of skin and systemic infections |
Table 10.5
![]()
- Why do inhibitors of bacterial nucleic acid synthesis not target host cells?
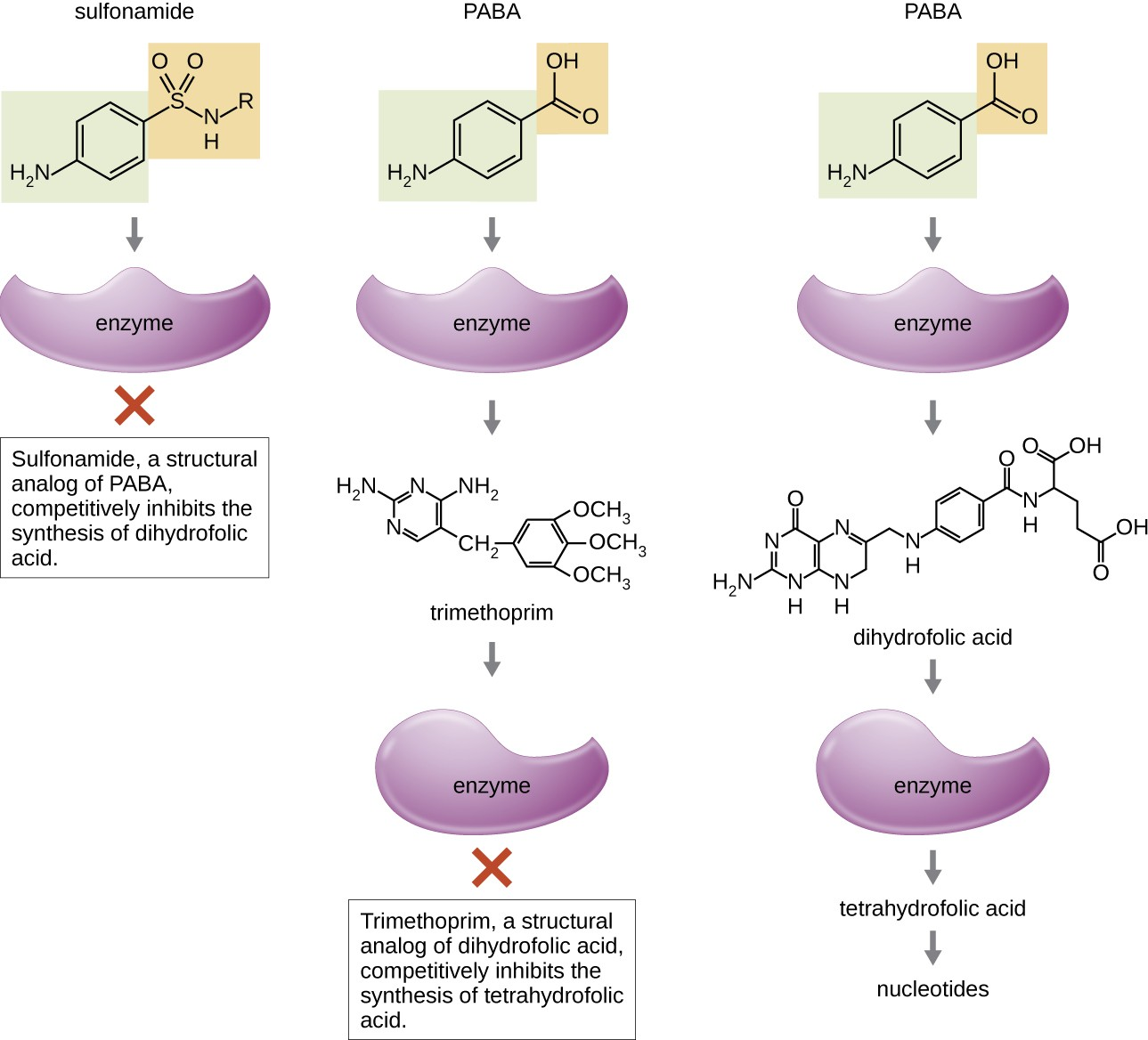
Inhibitors of Metabolic Pathways
Some synthetic drugs control bacterial infections by functioning as antimetabolites, competitive inhibitors for bacterial metabolic enzymes (Table 10.6). The sulfonamides (sulfa drugs) are the oldest synthetic antibacterial agents and are structural analogues of para-aminobenzoic acid (PABA), an early intermediate in folic acid synthesis (Figure 10.6). By inhibiting the enzyme involved in the production of dihydrofolic acid, sulfonamides block bacterial biosynthesis of folic acid and, subsequently, pyrimidines and purines required for nucleic acid synthesis. This mechanism of action provides bacteriostatic inhibition of growth against a wide spectrum of gram-positive and gram-negative pathogens. Because humans obtain folic acid from food instead of synthesizing it intracellularly, sulfonamides are selectively toxic for bacteria. However, allergic reactions to sulfa drugs are common. Another example of an antimetabolite that inhibits the folic acid synthesis pathway is trimethoprim, a synthetic antimicrobial compound (Figure 10.6). Trimethoprim is used in combination with the sulfa drug sulfamethoxazole to treat urinary tract infections, ear infections, and bronchitis. When used alone, each antimetabolite only decreases production of folic acid to a level where bacteriostatic inhibition of growth occurs. However, when used in combination, inhibition of both steps in the metabolic pathway decreases folic acid synthesis to a level that is lethal to the bacterial cell. Because of the importance of folic acid during fetal development, sulfa drugs and trimethoprim use should be carefully considered during early pregnancy.
|
Metabolic Pathway Target |
Mechanism of Action |
Drug Class |
Specific Drugs |
Spectrum of Activity |
|
Folic acid synthesis |
Inhibits the enzyme involved in production of dihydrofolic acid |
Sulfonamides |
Sulfamethoxazole |
Broad spectrum against gram-positive and gram- negative bacteria |
|
Sulfones |
Dapsone |
|||
|
Inhibits the enzyme involved in the production of tetrahydrofolic acid |
Not applicable |
Trimethoprim |
Broad spectrum against gram-positive and gram- negative bacteria |
Table 10.6
![]()
- How do sulfonamides and trimethoprim selectively target bacteria?
Inhibitor of ATP Synthase
Bedaquiline, representing the synthetic antibacterial class of compounds called the diarylquinolines, uses a novel mode of action that specifically inhibits mycobacterial growth. Although the specific mechanism has yet to be elucidated, this compound appears to interfere with the function of ATP synthases, perhaps by interfering with the use of the hydrogen ion gradient for ATP synthesis by oxidative phosphorylation, leading to reduced ATP production. Due to its side effects, including hepatotoxicity and potentially lethal heart arrhythmia, its use is reserved for serious, otherwise untreatable cases of tuberculosis.
Link to Learning
To learn more about the general principles of antimicrobial therapy and bacterial modes of action, visit Michigan State University’s Antimicrobial Resistance Learning Site (https://openstax.org/l/22MSUantireslea) , particularly pages 6 through 9.

