10.2 Integumentary Basic Concepts
Skin
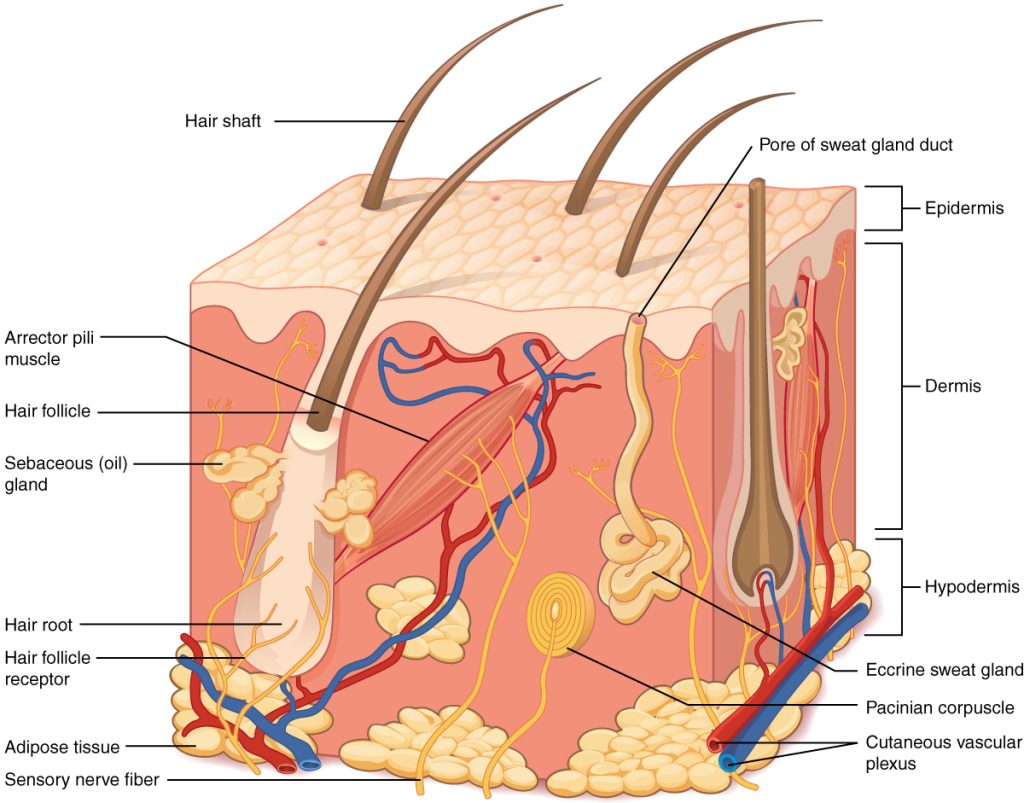
Skin is made up of three layers: epidermis, dermis, and hypodermis. See Figure 10.1[1] for an illustration of skin layers. The epidermis is the thin, topmost layer of the skin. It contains sweat gland duct openings and the visible part of hair known as the hair shaft. Underneath the epidermis lies the dermis where many essential components of skin function are located. The dermis contains hair follicles (the roots of hair shafts), sebaceous oil glands, blood vessels, endocrine sweat glands, and nerve endings. The bottommost layer of skin is the hypodermis (also referred to as the subcutaneous layer). It mostly consists of adipose tissue (fat), along with some blood vessels and nerve endings. Beneath the hypodermis layer lies bone, muscle, ligaments, and tendons.
There are several common skin disorders that a nurse may find when assessing a patient’s skin.
Hair
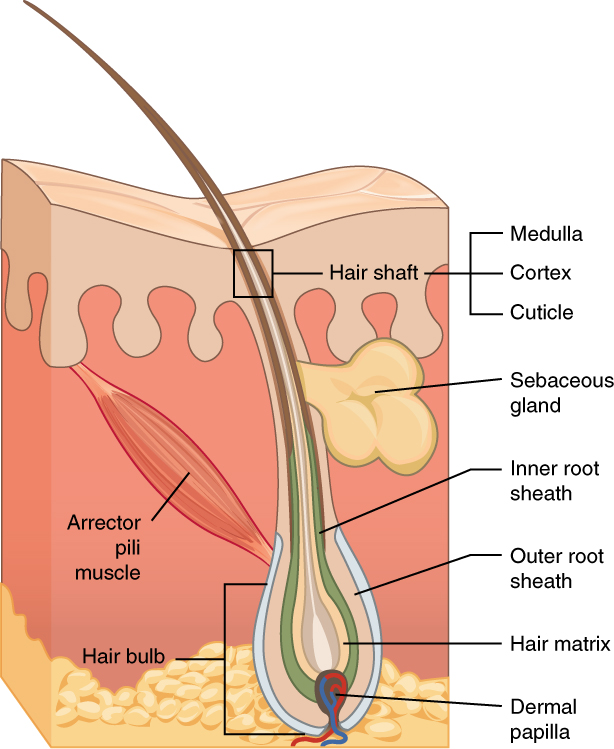
Hair is a filament that grows from a hair follicle in the dermis of the skin. See Figure 10.2[2] for an illustration of a hair follicle. It consists mainly of tightly packed, keratin-filled cells called keratinocytes. The human body is covered with hair follicles except for the mucous membranes, lips, palms of the hands, and soles of the feet. The part of the hair that is located within the follicle is called the hair root, the only living part of the hair. The part of the hair that is visible above the surface of the skin is the hair shaft. The shaft of the hair has no biochemical activity and is considered dead.
Functions of Hair
The functions of head hair are to provide insulation to retain heat and to protect the skin from damage by UV light. The function of hair in other locations on the body is debated. One idea is that body hair helps to keep us warm in cold weather. When the body is cold, the arrector pili muscles contract, causing hairs to stand up and trapping a layer of warm air above the epidermis. However, this action is more effective in mammals that have thick hair than it is in relatively hairless human beings.
Human hair has an important sensory function as well. Sensory receptors in the hair follicles can sense when the hair moves, whether it is because of a breeze or the touch of a physical object. Some hairs, such as the eyelashes, are especially sensitive to the presence of potentially harmful matter. The eyebrows protect the eyes from dirt, sweat, and rain. In addition, the eyebrows play a key role in nonverbal communication by expressing emotions such as sadness, anger, surprise, and excitement.[3]
Nails
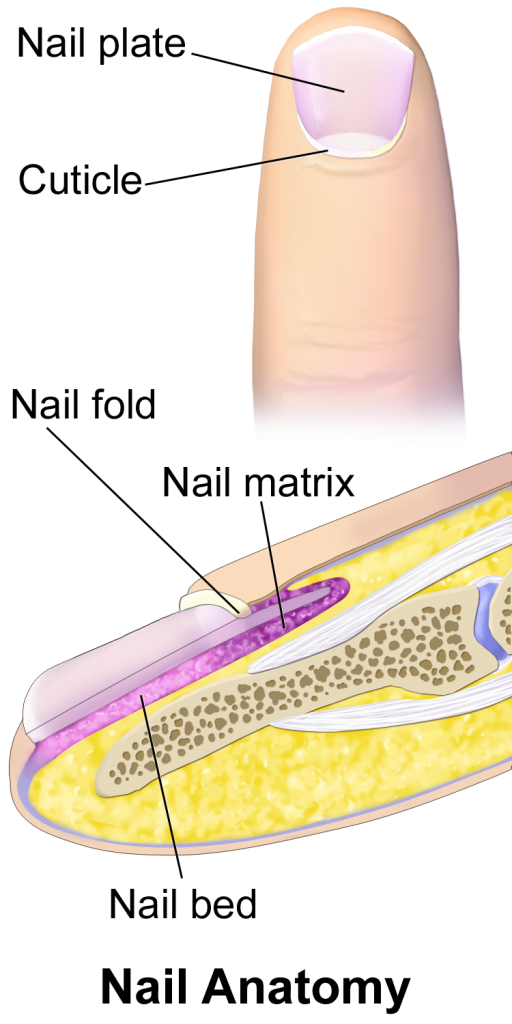
Nails are accessory organs of the skin. They are made of sheets of dead keratinocytes and are found on the distal ends of the fingers and toes. The keratin in nails makes them hard but flexible. Nails serve a number of purposes, including protecting the fingers, enhancing sensations, and acting like tools. A nail has three main parts: root, plate, and free margin. Other structures around or under the nail include the nail bed, cuticle, and nail fold. See Figure 10.3 for an illustration of the structure of a nail.[4],[5] The top diagram in this figure shows the external, visible part of the nail and the cuticle. The bottom diagram shows internal structures in a cross-section of the nail and nail bed.
Impaired Skin and Tissue Integrity
Skin integrity is a medical term that refers to skin health. Impaired skin integrity is a NANDA-I nursing diagnosis defined as, “Altered epidermis/or dermis.”[6] However, when deeper layers of the skin or integumentary structures are damaged, it is referred to as impaired tissue integrity. The NANDA-I definition of impaired tissue integrity is, “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.”[7]
Risk Factors Affecting Skin Health and Wound Healing
There are several risk factors that place a patient at increased risk for altered skin health and delayed wound healing. Risk factors include impaired circulation and oxygenation, impaired immune function, diabetes, inadequate nutrition, obesity, exposure to moisture, smoking, and age. Each of these risk factors is discussed in more detail in the following subsections.
Impaired Circulation and Oxygenation
Skin, like every other organ in the body, depends on good blood perfusion to keep it healthy and functioning correctly. Cardiovascular circulation delivers important oxygen, nutrients, infection-fighting cells, and clotting factors to tissues. These elements are needed by skin, tissues, and nerves to properly grow, function, and repair damage. Without good cardiovascular circulation, skin becomes damaged. Damage can occur from poor blood perfusion from the arteries, as well as from poor return of blood through the veins to the heart. Common medical conditions that decrease cardiovascular circulation include cardiac disease, diabetes, and peripheral vascular disease (PVD). PVD includes two medical conditions called arterial insufficiency and venous insufficiency.
Arterial Insufficiency
Arterial insufficiency refers to a lack of adequately oxygenated blood movement in arteries to specific tissues. Arterial insufficiency can be a sudden, acute lack of oxygenated blood, such as when a blood clot in an artery blocks blood flow to a specific area. Arterial insufficiency can also be a chronic condition caused by peripheral vascular disease (PVD). As a person’s arteries become blocked with plaque due to atherosclerosis, there is decreased blood flow to the tissues. Signs of arterial insufficiency are cool skin temperature, pale skin color, pain that increases with exercise, and possible arterial ulcers.
When oxygenated blood flow to tissues becomes inadequate, the tissue dies. This is called necrosis. Tissue death causes the skin and tissue to become necrotic (black). Necrotic tissue does not heal, so surgical debridement or amputation of the extremity becomes necessary for healing. See Figure 10.4[8] for images of an arterial insufficiency ulcer and necrotic toes.

Venous Insufficiency
Venous insufficiency occurs when the cardiovascular system cannot adequately return blood and fluid from the extremities to the heart. Venous insufficiency can cause stasis dermatitis when blood pools in the lower legs and leaks out into the skin and other tissues. Signs of venous insufficiency are edema, a brownish-leathery appearance to skin in the lower extremities, and venous ulcers that weep fluid.[9] See Figure 10.5[10] for an image of stasis dermatitis.

Impaired Immune Function
Skin contributes to the body’s immune function and is also affected by the immune system. Intact skin provides an excellent first line of defense against foreign objects entering the body. This is why it is essential to keep skin intact. If skin does break down, the next line of defense is a strong immune system that attacks harmful invading organisms. However, if the immune system is not working well, the body is much more susceptible to infections. This is why maintaining intact skin, especially in the presence of an impaired immune system, is imperative to decrease the risk of infections.
Stress can cause an impaired immune response that results in delayed wound healing.[11] Being hospitalized or undergoing surgery triggers the stress response in many patients. Medications, such as corticosteroids, also affect a patient’s immune function and can impair wound healing.[12] When assessing a chronic wound that is not healing as expected, it is important to consider the potential effects of stress and medications.
Diabetes
Diabetes can cause wounds to develop, as well as cause delayed wound healing. Nurses provide vital patient education to patients with diabetes to help them effectively manage the disease and prevent complications.
Read more about diabetes in the “Antidiabetics” section of the “Endocrine” chapter in Open RN Nursing Pharmacology.
Inadequate Nutrition
A healthy diet is essential for maintaining healthy skin, as well as maintaining an appropriate weight. Nutrients that are particularly important for skin health include protein; vitamins A, C, D, and E; and minerals such as selenium, copper, and zinc.[13]
Nutritional deficiencies can have a profound impact on wound healing and must be addressed for chronic wounds to heal. Protein is one of the most important nutritional factors affecting wound healing. For example, in patients with pressure injuries, 30 to 35 kcal/kg of calorie intake with 1.25 to 1.5g/kg of protein and micronutrients supplementation are recommended daily.[14] In addition, vitamin C and zinc have many roles in wound healing. It is important to collaborate with a dietician to identify and manage nutritional deficiencies when a patient is experiencing poor wound healing.[15]
Obesity
In the same way a balanced diet is vital for healthy skin, a healthy weight is also imperative. Obese individuals are at increased risk for fungal and yeast infections in skin folds caused by increased moisture and friction. See Figure 10.6[16] for an image of a fungal infection in the groin.[17] Symptoms of yeast and fungal infection include redness and scaliness of the skin associated with itching.

Obese patients also are at higher risk for wound complications due to a decreased supply of oxygenated blood flow to adipose tissue. Potential complications include infection, dehiscence (separation of the edges of a surgical wound), hematoma formation, pressure injuries, and venous ulcers.[18] Evisceration is a rare but severe complication when an abdominal surgical incision separates and the abdominal organs protrude or come out of the incision. Nurses can educate patients about making healthy lifestyle choices to reduce obesity and the risk of dehiscence. See Figure 10.7[19] for an image of a dehiscence in an abdominal surgical wound of an obese patient.

Exposure to Moisture
Healthy skin needs good moisture balance. If too much moisture (i.e., sweat, urine, or water) is left on the skin for extended periods of time, the skin will become soggy, wrinkly, and turn whiter than usual and is called maceration. A simple example of maceration is when you spend too much time in a bathtub and your fingers and toes turn white and get “pruny.” See Figure 10.8[20] for an image of maceration. If healthy skin is exposed to moisture for an extended period of time, such as when a moist wound dressing is incorrectly applied on healthy skin, the skin will break down. This type of skin breakdown is called excoriation. Excoriation refers to redness and removal of the topmost surface of the skin. See Figure 10.9[21] for an image of excoriation.


The opposite occurs when skin lacks proper moisture. Skin becomes flaky, itchy, and cracked when it becomes too dry. Conditions such as decreased moisture in the air during cold winter months or bathing in hot water can worsen skin dryness. Dry skin, especially when accompanied with cracking, breaks the protective barrier and increases the risk of infection. It is important for nurses to apply emollient cream to patients’ areas of dry skin to maintain the protective skin barrier.
Smoking
Smoking impacts the inflammatory phase of the wound healing process, which can result in poor wound healing and an increased risk of infection.[22] Patients who smoke should be encouraged to stop smoking.
Age
Older adults have thin, less elastic skin that is at increased risk for injury. They also have an altered inflammatory response that can impair wound healing. Nurses can educate older patients about the importance of exercise for skin health and improved wound healing as appropriate.[23]
- “501 Structure of the skin.jpg” by OpenStax is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/5-1-layers-of-the-skin ↵
- “506 Hair.jpg” by OpenStax is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/5-2-accessory-structures-of-the-skin. ↵
- This work is a derivative of Human Biology by Wakim and Grewal and is licensed under CC-BY-NC 4.0 ↵
- “Blausen_0406_FingerNailAnatomy.png” by BruceBlaus is licensed under CC BY 3.0 ↵
- This work is a derivative of Human Biology by Wakim and Grewal and is licensed under CC-BY-NC 4.0 ↵
- Herdman, T., & Kamitsuru, S. (2017). NANDA international nursing diagnoses: Definitions & classification 2018-2020 (11th ed.). Thieme Publishers. pp. 404, 406, 407, 412, 413. ↵
- Herdman, T., & Kamitsuru, S. (2017). NANDA international nursing diagnoses: Definitions & classification 2018-2020 (11th ed.). Thieme Publishers. pp. 404, 406, 407, 412, 413. ↵
- "JCCD147F1.gif” and “Infective-necrosis-of-second-toe_fig5_40484391” by unknown are licensed under CC BY 4.0 and CC BY-NC 4.0. Access for free at https://www.sciforschenonline.org/journals/clinical-cosmetic-dermatology/JCCD147.php and https://www.researchgate.net/figure/nfective-necrosis-of-second-toe_fig5_40484391 ↵
- Blackburn, L., Acree, K., Bartley, J., DiGiannantoni, E., Renner, E., & Sinnott, L. T. (2020). Microbial growth on the nails of direct patient care nurses wearing nail polish. Nursing Oncology Forum, 47(2), 155-164. https://doi.org/10.1188/20.onf.155-164 ↵
- ”3056fig1_opt.jpeg” by unknown is licensed under CC BY-NC 4.0. Access for free at https://www.medicaljournals.se/acta/content/html/10.2340/00015555-0692 ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier. pp. 348-349, 417-419. ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier. pp. 348-349, 417-419. ↵
- Park, K. (2015). Role of micronutrients in skin health and function. Biomolecules & Therapeutics, 23(3), 207–217. https://doi.org/10.4062/biomolther.2015.003 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10), 32-39. https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- “Tinea cruris.jpg” by Robertgascoin is licensed under CC BY-SA 3.0 ↵
- Rosen, T. (2011). Inframammary candida intertrigo. UpToDate. https://somepomed.org/articulos/contents/mobipreview.htm?0/29/474 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- “Bogota bag.png” by Suarez-Grau, J. M., Guadalajara Jurado, J. F., Gómez Menchero, J., & Bellido Luque, J. A. is licensed under CC BY 4.0 ↵
- “Trench_foot.jpg” by Mehmet Karatay is licensed under CC BY-SA 3.0 ↵
- “Dermatomyositis15.jpg” by Elizabeth M. Dugan, Adam M. Huber, Frederick W. Miller, and Lisa G. Rider is licensed under CC BY-SA 3.0 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
The very thin, top layer of the skin that contains openings of the sweat gland ducts and the visible part of hair known as the hair shaft.
The layer of skin underneath under the epidermis, containing hair follicles, sebaceous glands, blood vessels, endocrine sweat glands, and nerve endings.
The bottom layer of skin, also referred to as the subcutaneous layer, consisting mainly of adipose tissue or fat, along with some blood vessels and nerve endings. Beneath this layer lies muscle, tendons, ligaments, and bones.
Altered epidermis and/or dermis.
Damage to deeper layers of the skin or other integumentary structures. The NANDA-I definition of impaired tissue integrity is, “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.”
A condition caused by lack of adequately oxygenated blood supply to specific tissues.
Tissue death.
Dead tissue that is black.
A condition that occurs when the cardiovascular system cannot adequately return blood and fluid from the extremities to the heart.
Separation of the edges of a surgical wound.
A condition that occurs when skin has been exposed to moisture for too long causing it to appear soggy, wrinkled, or whiter than usual.
Redness and removal of the surface of the topmost layer of skin, often due to maceration or itching.

