4.4 Diagnosis
Open Resources for Nursing (Open RN)
Diagnosis is the second step of the nursing process (and the second Standard of Practice set by the American Nurses Association). This standard is defined as, “The registered nurse analyzes assessment data to determine actual or potential diagnoses, problems, and issues.” The RN “prioritizes diagnoses, problems, and issues based on mutually established goals to meet the needs of the health care consumer across the health–illness continuum and the care continuum.” Diagnoses, problems, strengths, and issues are documented in a manner that facilitates the development of expected outcomes and a collaborative plan.[1]
Analyzing Assessment Data
After collection of assessment data, the registered nurse analyzes the data to form generalizations and create hypotheses for nursing diagnoses. Steps for analyzing assessment data include performing data analysis, clustering of information, identifying hypotheses for potential nursing diagnosis, performing additional in-depth assessment as needed, and establishing nursing diagnosis statements. The nursing diagnoses are then prioritized and drive the nursing care plan.[2]
Performing Data Analysis
After nurses collect assessment data from a patient, they use their nursing knowledge to analyze that data to determine if it is “expected” or “unexpected” or “normal” or “abnormal” for that patient according to their age, development, and baseline status. From there, nurses determine what data are “clinically relevant” as they prioritize their nursing care.[3]
Example. In Scenario C in the “Assessment” section of this chapter, the nurse analyzes the vital signs data and determines the blood pressure, heart rate, and respiratory rate are elevated, and the oxygen saturation is decreased for this patient. These findings are considered “relevant cues.”
Clustering Information/Seeing Patterns/Making Hypotheses
After analyzing the data and determining relevant cues, the nurse clusters data into patterns. Assessment frameworks such as Gordon’s Functional Health Patterns assist nurses in clustering information according to evidence-based patterns of human responses. See the box below for an outline of Gordon’s Functional Health Patterns.[4] Concepts related to many of these patterns will be discussed in chapters later in this book.
Example. Refer to Scenario C of the “Assessment” section of this chapter. The nurse clusters the following relevant cues: elevated blood pressure, elevated respiratory rate, crackles in the lungs, weight gain, worsening edema, shortness of breath, a medical history of heart failure, and currently prescribed a diuretic medication. These cues are clustered into a generalization/pattern of fluid balance, which can be classified under Gordon’s Nutritional-Metabolic Functional Health Pattern. The nurse makes a hypothesis that the patient has excess fluid volume present.
Gordon’s Functional Health Patterns[5]
Health Perception-Health Management: A patient’s perception of their health and well-being and how it is managed
Nutritional-Metabolic: Food and fluid consumption relative to metabolic need
Elimination: Excretory function, including bowel, bladder, and skin
Activity-Exercise: Exercise and daily activities
Sleep-Rest: Sleep, rest, and daily activities
Cognitive-Perceptual: Perception and cognition
Self-perception and Self-concept: Self-concept and perception of self-worth, self-competency, body image, and mood state
Role-Relationship: Role engagements and relationships
Sexuality-Reproductive: Reproduction and satisfaction or dissatisfaction with sexuality
Coping-Stress Tolerance: Coping and effectiveness in terms of stress tolerance
Value-Belief: Values, beliefs (including spiritual beliefs), and goals that guide choices and decisions
Identifying Nursing Diagnoses
After the nurse has analyzed and clustered the data from the patient assessment, the next step is to begin to answer the question, “What are my patient’s human responses (i.e., nursing diagnoses)?” A nursing diagnosis is defined as, “A clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group, or community.”[6] Nursing diagnoses are customized to each patient and drive the development of the nursing care plan. The nurse should refer to a care planning resource and review the definitions and defining characteristics of the hypothesized nursing diagnoses to determine if additional in-depth assessment is needed before selecting the most accurate nursing diagnosis.
Nursing diagnoses are developed by nurses, for use by nurses. For example, NANDA International (NANDA-I) is a global professional nursing organization that develops nursing terminology that names actual or potential human responses to health problems and life processes based on research findings.[7] Currently, there are over 220 NANDA-I nursing diagnoses developed by nurses around the world. This list is continuously updated, with new nursing diagnoses added and old nursing diagnoses retired that no longer have supporting evidence. A list of commonly used NANDA-I diagnoses are listed in Appendix A. For a full list of NANDA-I nursing diagnoses, refer to a current nursing care plan reference.
NANDA-I nursing diagnoses are grouped into 13 domains that assist the nurse in selecting diagnoses based on the patterns of clustered data. These domains are similar to Gordon’s Functional Health Patterns and include health promotion, nutrition, elimination and exchange, activity/rest, perception/cognition, self-perception, role relationship, sexuality, coping/stress tolerance, life principles, safety/protection, comfort, and growth/development.
Nursing Diagnoses vs. Medical Diagnoses
You may be asking yourself, “How are nursing diagnoses different from medical diagnoses?” Medical diagnoses focus on diseases or other medical problems that have been identified by the physician, physician’s assistant, or advanced nurse practitioner. Nursing diagnoses focus on the human response to health conditions and life processes and are made independently by RNs. Patients with the same medical diagnosis will often respond differently to that diagnosis and thus have different nursing diagnoses. For example, two patients have the same medical diagnosis of heart failure. However, one patient may be interested in learning more information about the condition and the medications used to treat it, whereas another patient may be experiencing anxiety when thinking about the effects this medical diagnosis will have on their family. The nurse must consider these different responses when creating the nursing care plan. Nursing diagnoses consider the patient’s and family’s needs, attitudes, strengths, challenges, and resources as a customized nursing care plan is created to provide holistic and individualized care for each patient.
Example. A medical diagnosis identified for Ms. J. in Scenario C in the “Assessment” section is heart failure. This cannot be used as a nursing diagnosis, but it can be considered as an “associated condition” when creating hypotheses for nursing diagnoses. Associated conditions are medical diagnoses, injuries, procedures, medical devices, or pharmacological agents that are not independently modifiable by the nurse, but support accuracy in nursing diagnosis. The nursing diagnosis in Scenario C will be related to the patient’s response to heart failure.
Additional Definitions Used in NANDA-I Nursing Diagnoses
The following definitions of patient, age, and time are used in association with NANDA-I nursing diagnoses:
Patient
The NANDA-I definition of a “patient” includes:
- Individual: a single human being distinct from others (i.e., a person).
- Caregiver: a family member or helper who regularly looks after a child or a sick, elderly, or disabled person.
- Family: two or more people having continuous or sustained relationships, perceiving reciprocal obligations, sensing common meaning, and sharing certain obligations toward others; related by blood and/or choice.
- Group: a number of people with shared characteristics generally referred to as an ethnic group.
- Community: a group of people living in the same locale under the same governance. Examples include neighborhoods and cities.[8]
Age
The age of the person who is the subject of the diagnosis is defined by the following terms:[9]
- Fetus: an unborn human more than eight weeks after conception, until birth.
- Neonate: a person less than 28 days of age.
- Infant: a person greater than 28 days and less than 1 year of age.
- Child: a person aged 1 to 9 years
- Adolescent: a person aged 10 to 19 years
- Adult: a person older than 19 years of age unless national law defines a person as being an adult at an earlier age.
- Older adult: a person greater than 65 years of age.
Time
The duration of the diagnosis is defined by the following terms:[10]
- Acute: lasting less than 3 months.
- Chronic: lasting greater than 3 months.
- Intermittent: stopping or starting again at intervals
- Continuous: uninterrupted, going on without stop.
New Terms Used in 2018-2020 NANDA-I Diagnoses
The 2018-2020 edition of Nursing Diagnoses includes two new terms to assist in creating nursing diagnoses: at-risk populations and associated conditions.[11]
At-Risk Populations are groups of people who share a characteristic that causes each member to be susceptible to a particular human response, such as demographics, health/family history, stages of growth/development, or exposure to certain events/experiences.
Associated Conditions are medical diagnoses, injuries, procedures, medical devices, or pharmacological agents. These conditions are not independently modifiable by the nurse, but support accuracy in nursing diagnosis[12]
Types of Nursing Diagnoses
There are four types of NANDA-I nursing diagnoses:[13]
- Problem-Focused
- Health Promotion – Wellness
- Risk
- Syndrome
A problem-focused nursing diagnosis is a “clinical judgment concerning an undesirable human response to health condition/life processes that exist in an individual, family, group, or community.”[14] To make an accurate problem-focused diagnosis, related factors and defining characteristics must be present. Related factors (also called etiology) are causes that contribute to the diagnosis. Defining characteristics are cues, signs, and symptoms that cluster into patterns.[15]
A health promotion-wellness nursing diagnosis is “a clinical judgment concerning motivation and desire to increase well-being and to actualize human health potential.” These responses are expressed by the patient’s readiness to enhance specific health behaviors.[16]A health promotion-wellness diagnosis is used when the patient is willing to improve a lack of knowledge, coping, or other identified need.
A risk nursing diagnosis is “a clinical judgment concerning the vulnerability of an individual, family, group, or community for developing an undesirable human response to health conditions/life processes.”[17] A risk nursing diagnosis must be supported by risk factors that contribute to the increased vulnerability. A risk nursing diagnosis is different from the problem-focused diagnosis in that the problem has not yet actually occurred. Problem diagnoses should not be automatically viewed as more important than risk diagnoses because sometimes a risk diagnosis can have the highest priority for a patient.[18]
A syndrome diagnosis is a “clinical judgment concerning a specific cluster of nursing diagnoses that occur together, and are best addressed together and through similar interventions.”[19]
Establishing Nursing Diagnosis Statements
When using NANDA-I nursing diagnoses, NANDA-I recommends the structure of a nursing diagnosis should be a statement that includes the nursing diagnosis and related factors as exhibited by defining characteristics. The accuracy of the nursing diagnosis is validated when a nurse is able to clearly link the defining characteristics, related factors, and/or risk factors found during the patient’s assessment.[20]
To create a nursing diagnosis statement, the registered nurse completes the following steps. After analyzing the patient’s subjective and objective data and clustering the data into patterns, the nurse generates hypotheses for nursing diagnoses based on how the patterns meet defining characteristics of a nursing diagnosis. Defining characteristics is the terminology used for observable signs and symptoms related to a nursing diagnosis.[21] Defining characteristics are included in care planning resources for each nursing diagnosis, along with a definition of that diagnosis, so the nurse can select the most accurate diagnosis. For example, objective and subjective data such as weight, height, and dietary intake can be clustered together as defining characteristics for the nursing diagnosis of nutritional status.
When creating a nursing diagnosis statement, the nurse also identifies the cause of the problem for that specific patient. Related factors is the terminology used for the underlying causes (etiology) of a patient’s problem or situation. Related factors should not be a medical diagnosis, but instead should be attributed to the underlying pathophysiology that the nurse can treat. When possible, the nursing interventions planned for each nursing diagnosis should attempt to modify or remove these related factors that are the underlying cause of the nursing diagnosis.[22]
Creating nursing diagnosis statements has traditionally been referred to as “using PES format.” The PES mnemonic no longer applies to the current terminology used by NANDA-I, but the components of a nursing diagnosis statement remain the same. A nursing diagnosis statement should contain the problem, related factors, and defining characteristics. These terms fit under the former PES format in this manner:
Problem (P) – the patient problem (i.e., the nursing diagnosis)
Etiology (E) – related factors (i.e., the etiology/cause) of the nursing diagnosis; phrased as “related to” or “R/T”
Signs and Symptoms (S) – defining characteristics manifested by the patient (i.e., the signs and symptoms/subjective and objective data) that led to the identification of that nursing diagnosis for the patient; phrased with “as manifested by” or “as evidenced by.”
Examples of different types of nursing diagnoses are further explained below.
Problem-Focused Nursing Diagnosis
A problem-focused nursing diagnosis contains all three components of the PES format:
Problem (P) – statement of the patient response (nursing diagnosis)
Etiology (E) – related factors contributing to the nursing diagnosis
Signs and Symptoms (S) – defining characteristics manifested by that patient
Sample Problem-Focused Nursing Diagnosis Statement
Refer to Scenario C of the “Assessment” section of this chapter. The cluster of data for Ms. J. (elevated blood pressure, elevated respiratory rate, crackles in the lungs, weight gain, worsening edema, and shortness of breath) are defining characteristics for the NANDA-I Nursing Diagnosis Excess Fluid Volume. The NANDA-I definition of Excess Fluid Volume is “surplus intake and/or retention of fluid.” The related factor (etiology) of the problem is that the patient has excessive fluid intake.[23]
Example
The components of a problem-focused nursing diagnosis statement for Ms. J. would be:
(P) Fluid Volume Excess
(E) Related to excessive fluid intake
(S) As manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, increased weight of 10 pounds, and the patient reports, “My ankles are so swollen.”
A correctly written problem-focused nursing diagnosis statement for Ms. J. would look like this:
Fluid Volume Excess related to excessive fluid intake as manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, an increase weight of 10 pounds, and the patient reports, “My ankles are so swollen.”
Health-Promotion Nursing Diagnosis
A health-promotion nursing diagnosis statement contains the problem (P) and the defining characteristics (S). The defining characteristics component of a health-promotion nursing diagnosis statement should begin with the phrase “expresses desire to enhance”:[24]
Problem (P) – statement of the patient response (nursing diagnosis)
Signs and Symptoms (S) – the patient’s expressed desire to enhance
Sample Health-Promotion Nursing Diagnosis Statement
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. demonstrates a readiness to improve her health status when she told the nurse that she would like to “learn more about my health so I can take better care of myself.” This statement is a defining characteristic of the NANDA-I nursing diagnosis Readiness for Enhanced Health Management, which is defined as “a pattern of regulating and integrating into daily living a therapeutic regimen for the treatment of illness and its sequelae, which can be strengthened.”[25]
Example
The components of a health-promotion nursing diagnosis for Ms. J. would be:
Problem (P): Readiness for Enhanced Health Management
Symptoms (S): Expressed desire to “learn more about my health so I can take better care of myself.”
A correctly written health-promotion nursing diagnosis statement for Ms. J. would look like this:
Enhanced Readiness for Health Promotion as manifested by expressed desire to “learn more about my health so I can take better care of myself.”
Risk Nursing Diagnosis
A risk nursing diagnosis should be supported by evidence of the patient’s risk factors for developing that problem. Different experts recommend different phrasing. NANDA-I 2018-2020 recommends using the phrase “as evidenced by” to refer to the risk factors for developing that problem.[26]
A risk diagnosis consists of the following:
Problem (P) – statement of the patient response (nursing diagnosis)
As Evidenced By – Risk factors for developing the problem
Sample Risk Diagnosis Statement
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. has an increased risk of falling due to vulnerability from the dizziness and weakness she is experiencing. The NANDA-I definition of Risk for Falls is “increased susceptibility to falling, which may cause physical harm and compromise health.”[27]
Example
The components of a risk diagnosis statement for Ms. J. would be:
Problem (P) – Risk for Falls
As Evidenced By – Dizziness and decreased lower extremity strength
A correctly written risk nursing diagnosis statement for Ms. J. would look like this:
Risk for Falls as evidenced by dizziness and decreased lower extremity strength.
Syndrome Diagnosis
A syndrome is a cluster of nursing diagnoses that occur together and are best addressed together and through similar interventions. To create a syndrome diagnosis, two or more nursing diagnoses must be used as defining characteristics (S) that create a syndrome. Related factors may be used if they add clarity to the definition, but are not required.[28]
A syndrome statement consists of these items:
Problem (P) – the syndrome
Signs and Symptoms (S) – the defining characteristics are two or more similar nursing diagnoses
Sample Syndrome Diagnosis Statement
Refer to Scenario C in the “Assessment” section of this chapter. Clustering the data for Ms. J. identifies several similar NANDA-I nursing diagnoses that can be categorized as a syndrome. For example, Activity Intolerance is defined as “insufficient physiological or psychological energy to endure or complete required or desired daily activities.” Social Isolation is defined as “aloneness experienced by the individual and perceived as imposed by others and as a negative or threatening state.” These diagnoses can be included under the the NANDA-I syndrome named Risk for Frail Elderly Syndrome. This syndrome is defined as a “dynamic state of unstable equilibrium that affects the older individual experiencing deterioration in one or more domains of health (physical, functional, psychological, or social) and leads to increased susceptibility to adverse health effects, in particular disability.”[29]
Example
The components of a syndrome nursing diagnosis for Ms. J. would be:
(P) – Risk for Frail Elderly Syndrome
(S) – The nursing diagnoses of Activity Intolerance and Social Isolation
Additional related factor: Fear of falling
A correctly written syndrome diagnosis statement for Ms. J. would look like this:
Risk for Frail Elderly Syndrome related to activity intolerance, social isolation, and fear of falling
Prioritization
After identifying nursing diagnoses, the next step is prioritization according to the specific needs of the patient. Nurses prioritize their actions while providing patient care multiple times every day. Prioritization is the process that identifies the most significant nursing problems, as well as the most important interventions, in the nursing care plan.
It is essential that life-threatening concerns and crises are identified immediately and addressed quickly. Depending on the severity of a problem, the steps of the nursing process may be performed in a matter of seconds for life-threatening concerns. In critical situations, the steps of the nursing process are performed through rapid clinical judgment. Nurses must recognize cues signaling a change in patient condition, apply evidence-based practices in a crisis, and communicate effectively with interprofessional team members. Most patient situations fall somewhere between a crisis and routine care.
There are several concepts used to prioritize, including Maslow’s Hierarchy of Needs, the “ABCs” (Airway, Breathing and Circulation), and acute, uncompensated conditions. See the infographic in Figure 4.7[30] on The How To of Prioritization.

Maslow’s Hierarchy of Needs is used to categorize the most urgent patient needs. The bottom levels of the pyramid represent the top priority needs of physiological needs intertwined with safety. See Figure 4.8[31] for an image of Maslow’s Hierarchy of Needs. You may be asking yourself, “What about the ABCs – isn’t airway the most important?” The answer to that question is “it depends on the situation and the associated safety considerations.” Consider this scenario – you are driving home after a lovely picnic in the country and come across a fiery car crash. As you approach the car, you see that the passenger is not breathing. Using Maslow’s Hierarchy of Needs to prioritize your actions, you remove the passenger from the car first due to safety even though he is not breathing. After ensuring safety and calling for help, you follow the steps to perform cardiopulmonary resuscitation (CPR) to establish circulation, airway, and breathing until help arrives.
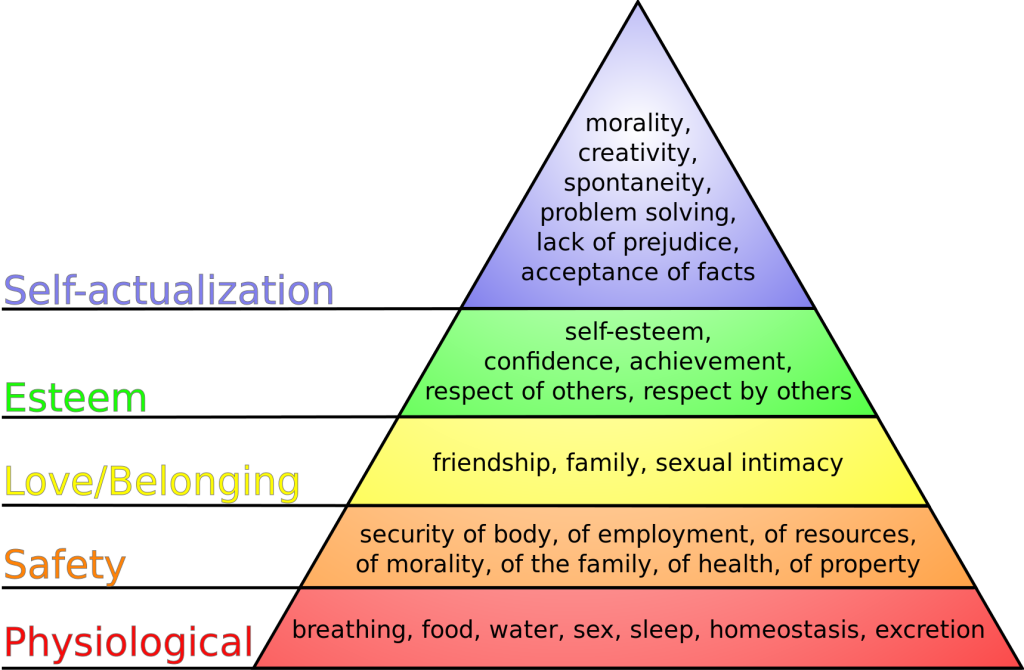
In addition to using Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation, the nurse also considers if the patient’s condition is an acute or chronic problem. Acute, uncompensated conditions generally require priority interventions over chronic conditions. Additionally, actual problems generally receive priority over potential problems, but risk problems sometimes receive priority depending on the patient vulnerability and risk factors.
Example. Refer to Scenario C in the “Assessment” section of this chapter. Four types of nursing diagnoses were identified for Ms. J.: Fluid Volume Excess, Enhanced Readiness for Health Promotion, Risk for Falls, and Risk for Frail Elderly Syndrome. The top priority diagnosis is Fluid Volume Excess because it affects the physiological needs of breathing, homeostasis, and excretion. However, the Risk for Falls diagnosis comes in a close second because of safety implications and potential injury that could occur if the patient fell.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Gordon, M. (2008). Assess notes: Nursing assessment and diagnostic reasoning. F.A. Davis Company. ↵
- Gordon, M. (2008). Assess notes: Nursing assessment and diagnostic reasoning. F.A. Davis Company. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- “The How To of Prioritization” by Valerie Palarski for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Maslow's hierarchy of needs.svg” by J. Finkelstein is licensed under CC BY-SA 3.0 ↵
Learning Objectives
- Outline the factors that put patients at risk for infection
- Identify factors related to infection across the life span
- Outline personal practices that reduce the risk of infection transmission
- Base your care decision on the signs and symptoms of infection
- Base your response on an interpretation of the diagnostic tests related to patient's infectious process
- Detail the nursing interventions to support or minimize the physical and psychological effects of the infectious process
- Demonstrate the ability to correlate nursing interventions to methods used to prevent or disrupt the chain of infection
- Follow industry standards for transmission-based precautions
- Identify evidence-based practices
Have you ever wondered how nurses can be exposed to patients with communicable diseases day after day and not become ill? There are many factors that affect the body’s ability to defend against infection and place some individuals at greater risk of developing an infection. When an infection does occur, early recognition is important to prevent it from spreading within the individual, as well as to others. Protecting people from developing an infection, as well as preventing the spread of infection, is a major concern for nurses. This chapter will discuss the physiology of the inflammation and infectious processes and nursing interventions to prevent the spread of infection.
Normal Flora and Microbiome
Microorganisms occur naturally and are present everywhere in our environment. Some microorganisms live on the skin, in the nasopharynx, and in the gastrointestinal tract, but don’t become an infection unless the host becomes susceptible. These microorganisms are called normal flora . Over the past several years, it has been discovered that every human being carries their own individual suite of microorganisms in and on their body referred to as their microbiome. A person's microbiome is acquired at birth and evolves over their lifetime. It is different across body sites and between individuals. A person's gut microbiome has recently been found to impact their immune system.[1],[2]
Pathogens
Microorganisms that cause disease are called pathogens. There are four common types of pathogens, including viruses, bacteria, fungi, and parasites.
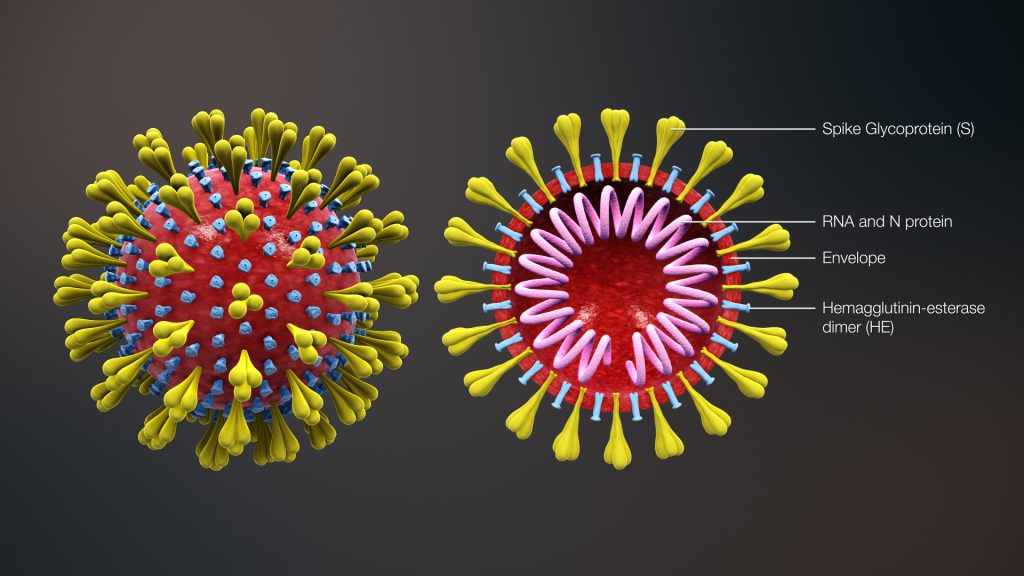
Viruses
Viruses are made up of a piece of genetic code, such as DNA or RNA, and are protected by a coating of protein. After a host (i.e., the person) becomes infected by a virus, the virus invades the body’s cells and uses the components of the cell to replicate and produce more viruses. After the virus replication cycle is complete, the new viruses are released into the body, causing damage or destruction of the host’s cells.[3]
Antiviral medications can be used to treat some viral infections. Antibiotics do not kill viruses and are ineffective as a treatment for viral infections. See Figure 9.1[4] for an image of a virus.
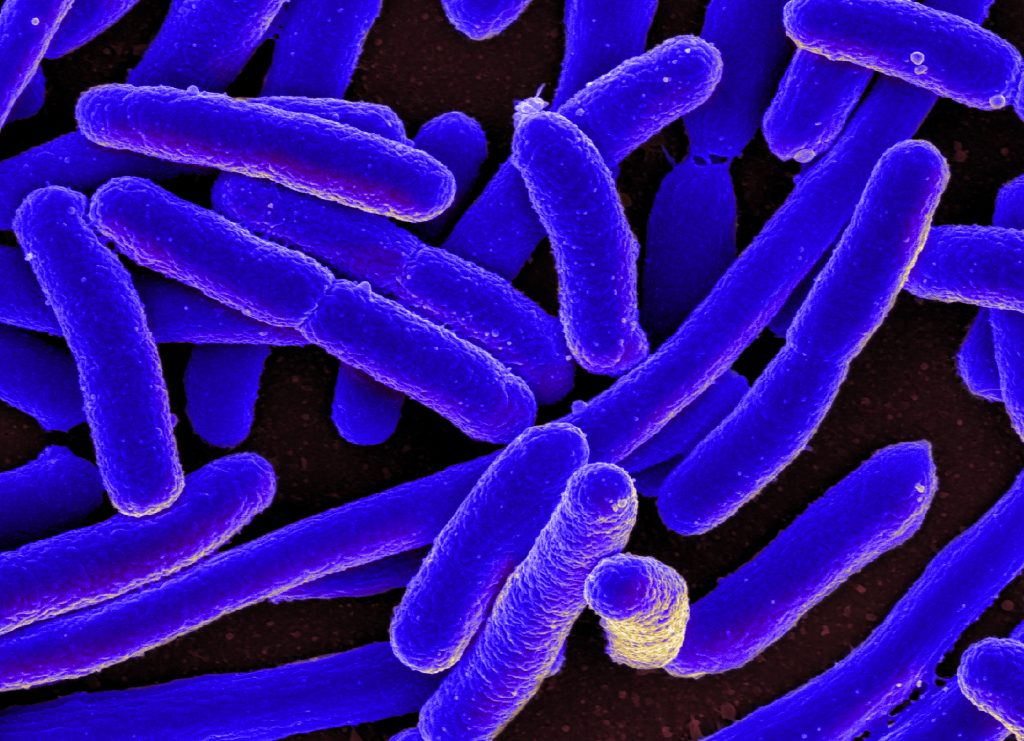
Bacteria
Bacteria are microorganisms made of a single cell. They are very diverse, have a variety of shapes and features, and have the ability to live in any environment, including your body. However, not all bacteria cause infections. Those that cause infection are called pathogenic bacteria. See Figure 9.2[5] for an image of a bacterium called Escherichia coli (E. coli).
A patient is susceptible to bacterial infections when their immune system is compromised by chronic diseases or certain types of medications. Antibiotics are used to treat bacterial infections. However, some strains of bacteria have become resistant to antibiotics, making them difficult to treat. For example, infections caused by methicillin-resistant Staphylococcus Aureus (MRSA) are resistant to many types of antibiotics and have the capability of producing severe and life-threatening infections. MRSA infections usually require IV antibiotics and may require treatment for long periods of time.[6]
Fungi
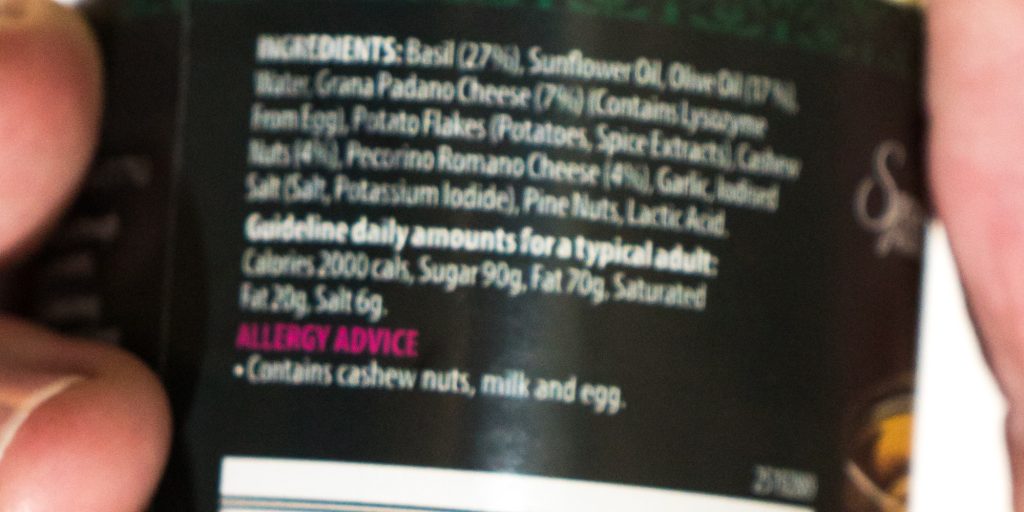
There are millions of different fungal species on Earth. Fungi can be found everywhere in the environment, including indoors, outdoors, and on human skin, but only about 300 species cause infection when they overgrow. Candida albicans is a type of fungus that can cause oral thrush and vaginal yeast infections, especially in susceptible patients or those taking antibiotics.[7] See Figure 9.3[8] for an image of oral thrush.
Fungi cells contain a nucleus and other components protected by a membrane and a thick cell wall. This structure can make them harder to kill. Some new strains of fungal infections are proving to be especially dangerous, such as Candida auris, which is difficult to diagnose and treat, and can cause outbreaks in health care facilities.[9]

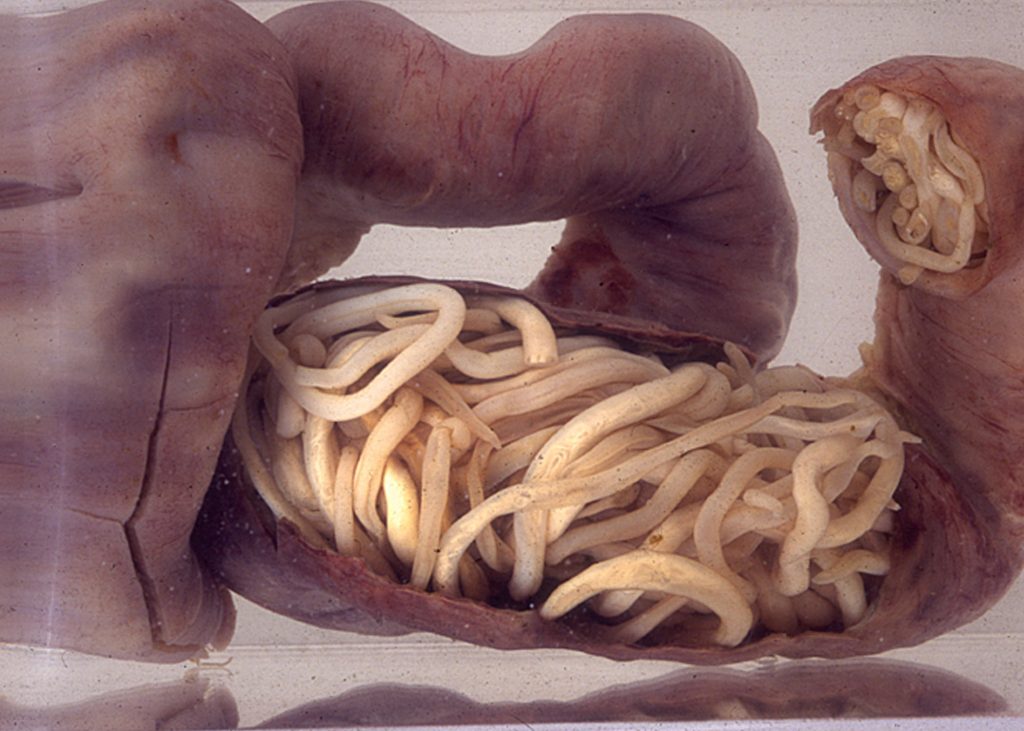
Parasites
Parasites are organisms that behave like tiny animals, living in or on a host, and feeding at the expense of the host. Three main types of parasites can cause disease in humans. These include the following:
- Protozoa: Single-celled organisms that can live and multiply in your body
- Helminths: Multi-celled organisms that can live inside or outside your body and are commonly known as worms
- Ectoparasites: Multi-celled organisms that live on or feed off skin, including ticks and mosquitos
Parasites can be spread several ways, including through contaminated soil, water, food, and blood, as well as through sexual contact and insect bites.[10] See Figure 9.4[11] for an image of a helminth infection causing intestinal obstruction in a child.
Adult day centers: Care that offers people with dementia and other chronic illnesses the opportunity to be social and to participate in activities in a safe environment, while also giving their caregivers the opportunity to work, run errands, or take a much-needed break.
Ageism: The stereotyping and discrimination against individuals or groups on the basis of their age. Ageism can take many forms, including prejudicial attitudes, discriminatory practices, or institutional policies and practices that perpetuate stereotypical beliefs.
Alzheimer’s disease: An irreversible, progressive brain disorder that slowly destroys memory and thinking skills and eventually the ability to carry out the simplest tasks.
Cognition: A term used to describe our ability to think.
Cognitive impairment: Impairment in mental processes that drive how an individual understands and acts in the world, affecting the acquisition of information and knowledge.
Delirium: An acute state of cognitive impairment that typically occurs suddenly due to a physiological cause, such as infection, hypoxia, electrolyte imbalances, drug effects, or other acute brain injury.
Dementia: A chronic condition of impaired cognition, caused by brain disease or injury, marked by personality changes, memory deficits, and impaired reasoning. Dementia can be caused by a group of conditions, such as Alzheimer’s disease, vascular dementia, frontal-temporal dementia, and Lewy body disease. It is gradual, progressive, and irreversible.
Depression: A brain disorder with a variety of causes, including genetic, biological, environmental, and psychological factors.
Development: Biological changes, as well as social and cognitive changes, that occur continuously throughout our lives.
Growth: Physical changes that occur during the development of an individual beginning at the time of conception.
Hospice care: Care that focuses on providing comfort and dignity at the end of life. It involves care and support services that can be of great benefit to people in the final stages of dementia and to their families.
Intellectual disability: A diagnostic term that describes intellectual and adaptive functioning deficits identified during the developmental period prior to the age 18.
Respite care: Care provided at home (by a volunteer or paid service) or in a care setting, such as adult day centers or residential facilities, that allows the caregiver to take a much-needed break.
Sundowning: Increased confusion, anxiety, agitation, pacing, or disorientation in patients with dementia that typically begins at dusk and continues throughout the night.
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
- You are providing care for Mrs. Jones, an 83-year-old female patient admitted to the medical surgical floor with worsening pneumonia. Upon auscultation of the patient's lung fields, you note scattered crackles and diminished breath sounds throughout all lung fields. Mrs. Jones requires 4L O2 via nasal cannula to maintain an oxygen saturation of 94%. You have constructed a nursing care diagnosis of Ineffective Breathing Pattern. What nursing interventions might you consider to help improve the patient's breathing pattern?
Apnea: Temporary cessation of breathing. When apnea occurs during sleep, it is often caused by the condition called Obstructive Sleep Apnea (OSA).
Arterial Blood Gas (ABG): Diagnostic test performed on an arterial sample of blood to determine its pH level, oxygenation status, and carbon dioxide status.
Barrel chest: An increased anterior-posterior chest diameter, resulting from air trapping in the alveoli, that occurs in chronic respiratory disease.
Bilevel Positive Airway Pressure (BiPAP): A BiPAP is an oxygenation device similar to a CPAP device in its use to prevent airways from collapsing, but it has two pressure settings. One setting occurs during inhalation and a lower pressure setting is used during exhalation. BiPAP devices may be used in the home to treat obstructive sleep apnea or in hospitals to treat patients in acute respiratory distress. For more information, see the “Oxygenation Equipment” section of the "Oxygen Therapy" chapter in Open RN Nursing Skills.
Bradypnea: Decreased respiratory rate less than the normal range according to the patient’s age.
Cardiac output: The amount of blood the heart pumps in one minute.
Continuous Positive Airway Pressure (CPAP): A CPAP is an oxygenation device is typically used for patients who are able to breath spontaneously but need assistance in keeping their airway unobstructed, such as those with obstructive sleep apnea. The CPAP device consists of a mask that covers the patient's nose, or nose and mouth, and is attached to a machine that continuously applies mild air pressure to keep the airways from collapsing. For more information, see the “Oxygenation Equipment” section of the "Oxygen Therapy" chapter in Open RN Nursing Skills.
Clubbing: Enlargement of the fingertips that occurs with chronic hypoxia.
Coughing and deep breathing: A breathing technique where the patient is encouraged to take deep, slow breaths and then exhale slowly. After each set of breaths, the patient should cough. This technique is repeated 3 to 5 times every hour.
Cyanosis: Bluish discoloration of the skin and mucous membranes.
Dyspnea: A subjective feeling of not getting enough air. Depending on severity, dyspnea causes increased levels of anxiety.
Endotracheal Tube (ET tube): An ET tube is inserted by an advanced practitioner to maintain a secure airway when a patient is experiencing respiratory failure or is receiving general anesthesia. For more information, see the “Oxygenation Equipment” section of the "Oxygen Therapy" chapter in Open RN Nursing Skills.
HCO3: Bicarbonate level of arterial blood indicated in an arterial blood gas (ABG) result. Normal range is 22-26.
Huffing technique: A technique helpful for patients who have difficulty coughing. Teach the patient to inhale with a medium-sized breath and then make a sound like “ha” to push the air out quickly with the mouth slightly open.
Hypercapnia: Elevated level of carbon dioxide in the blood.
Hypoxemia: A specific type of hypoxia that is defined as decreased partial pressure of oxygen in the blood (PaO2) indicated in an arterial blood gas (ABG) result.
Hypoxia: A reduced level of tissue oxygenation. Hypoxia has many causes, ranging from respiratory and cardiac conditions to anemia.
Incentive spirometer: A medical device commonly prescribed after surgery to reduce the buildup of fluid in the lungs and to prevent pneumonia. While sitting upright, the patient should breathe in slowly and deeply through the tubing with the goal of raising the piston to a specified level. The patient should attempt to hold their breath for 5 seconds, or as long as tolerated, and then rest for a few seconds. This technique should be repeated by the patient 10 times every hour while awake.
Mechanical ventilator: A mechanical ventilator is a machine attached to an endotracheal tube to assist or replace spontaneous breathing. For more information, see the “Oxygenation Equipment” section of the "Oxygen Therapy" chapter in Open RN Nursing Skills.
Orthopnea: Difficulty in breathing that occurs when lying down and is relieved upon changing to an upright position.
PaCO2: Partial pressure of carbon dioxide level in arterial blood indicated in an ABG result. Normal range is 35-45 mmHg.
PaO2: Partial pressure of oxygen level in arterial blood indicated in an ABG result. Normal range is 80-100 mmHg.
Perfusion: The passage of blood through the arteries to an organ or tissue.
Pursed-lip breathing: A breathing technique that encourages a person to inhale through the nose and exhale through the mouth at a slow, controlled flow.
Purulent sputum: Yellow or green sputum that often indicates a respiratory infection.
Respiration: Gas exchange occurs at the alveolar level where blood is oxygenated and carbon dioxide is removed.
SaO2: Calculated oxygen saturation level in an ABG result. Normal range is 95-100%.
SpO2: Hemoglobin saturation level measured by pulse oximetry. Normal range is 94-98%.
Sputum: Mucus and other secretions that are coughed up from the mouth.
Tachypnea: Elevated respiratory rate above normal range according to the patient’s age.
Tripod position: A position that enhances air exchange when a patient sits up and leans over by resting their arms on their legs or on a bedside table; also referred to as a three-point position.
Ventilation: Mechanical movement of air into and out of the lungs.
Vibratory Positive Expiratory Pressure (PEP) Therapy: Handheld devices such as flutter valves or Acapella devices used with patients who need assistance in clearing mucus from their airways.
Adult day centers: Care that offers people with dementia and other chronic illnesses the opportunity to be social and to participate in activities in a safe environment, while also giving their caregivers the opportunity to work, run errands, or take a much-needed break.
Ageism: The stereotyping and discrimination against individuals or groups on the basis of their age. Ageism can take many forms, including prejudicial attitudes, discriminatory practices, or institutional policies and practices that perpetuate stereotypical beliefs.
Alzheimer’s disease: An irreversible, progressive brain disorder that slowly destroys memory and thinking skills and eventually the ability to carry out the simplest tasks.
Cognition: A term used to describe our ability to think.
Cognitive impairment: Impairment in mental processes that drive how an individual understands and acts in the world, affecting the acquisition of information and knowledge.
Delirium: An acute state of cognitive impairment that typically occurs suddenly due to a physiological cause, such as infection, hypoxia, electrolyte imbalances, drug effects, or other acute brain injury.
Dementia: A chronic condition of impaired cognition, caused by brain disease or injury, marked by personality changes, memory deficits, and impaired reasoning. Dementia can be caused by a group of conditions, such as Alzheimer’s disease, vascular dementia, frontal-temporal dementia, and Lewy body disease. It is gradual, progressive, and irreversible.
Depression: A brain disorder with a variety of causes, including genetic, biological, environmental, and psychological factors.
Development: Biological changes, as well as social and cognitive changes, that occur continuously throughout our lives.
Growth: Physical changes that occur during the development of an individual beginning at the time of conception.
Hospice care: Care that focuses on providing comfort and dignity at the end of life. It involves care and support services that can be of great benefit to people in the final stages of dementia and to their families.
Intellectual disability: A diagnostic term that describes intellectual and adaptive functioning deficits identified during the developmental period prior to the age 18.
Respite care: Care provided at home (by a volunteer or paid service) or in a care setting, such as adult day centers or residential facilities, that allows the caregiver to take a much-needed break.
Sundowning: Increased confusion, anxiety, agitation, pacing, or disorientation in patients with dementia that typically begins at dusk and continues throughout the night.
Learning Objectives
- Collect data to identify patients experiencing alterations in sensory perception
- Identify factors related to sensory impairments across the life span
- Demonstrate respect for the dignity of the patient with a sensory impairment
- Detail support for family/significant others caring for patients with a sensory impairment
- Include community resources available for patients and families with a sensory impairment
- Include adaptations to the environment to maintain safety for the patient with a sensory impairment
- Incorporate nursing strategies to maximize sensory perception
- Outline nursing interventions for specific sensory disorders
- Identify evidence-based practices
Our five basic senses of sight (vision), hearing (auditory), touch (tactile), smell (olfactory), and taste (gustatory) help us perceive and act in the world around us. See Figure 7.1[12] for an illustration of our five senses.
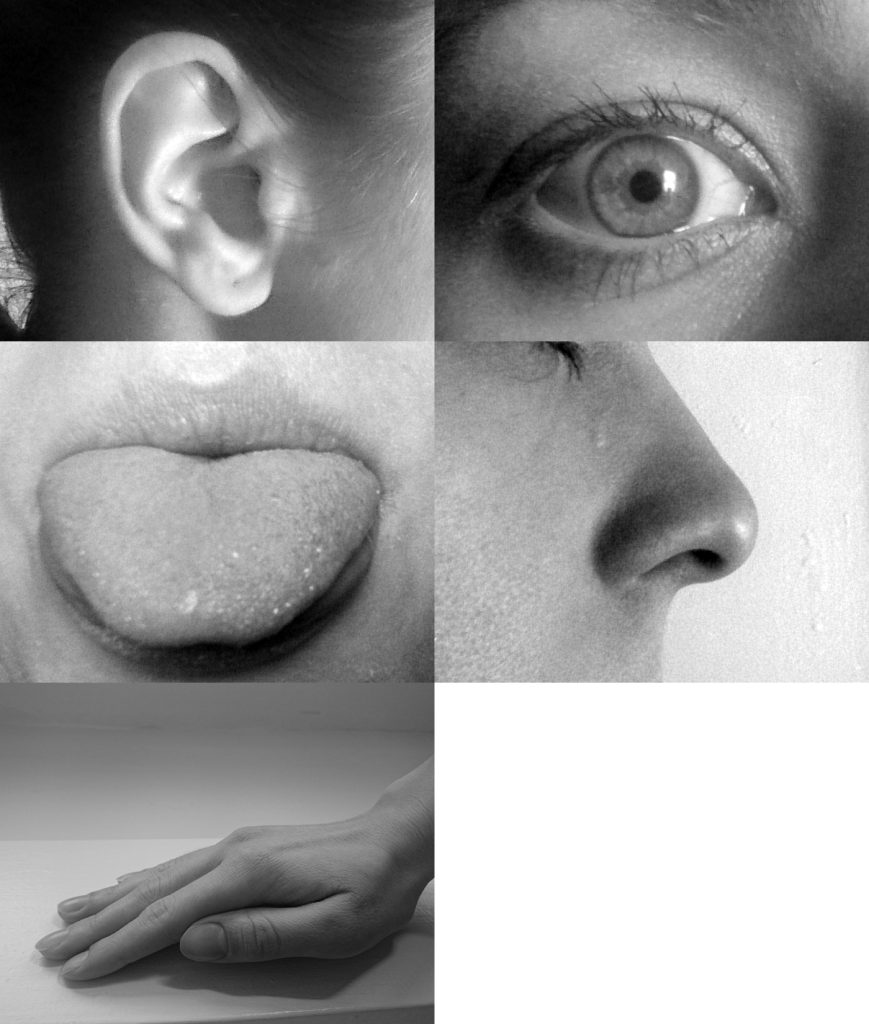
We may not often consider the importance of our sensory input. As nurses, we especially rely on our senses when providing patient care as we gather assessment data. We ask questions and listen to patient responses, we listen to their heart and lung sounds, we evaluate the appearance of their skin, we may smell an infectious process when changing a wound dressing, and we feel the sensation of pulses when assessing circulation.
When an individual experiences sensory impairment because of the loss of one or more senses or is affected by the amount of stimuli (too much or too little), their ability to safely function is impacted. Nurses identify patients’ sensory impairments and implement interventions to improve their safety, functioning, and quality of life. The nurse’s goal is to provide support and dignity to individuals and their families by using strategies and resources that will help them to engage with their surroundings and others to the best of their ability.
This chapter will review common sensory impairments and related nursing care.
Learning Objectives
- Collect data to identify patients experiencing alterations in sensory perception
- Identify factors related to sensory impairments across the life span
- Demonstrate respect for the dignity of the patient with a sensory impairment
- Detail support for family/significant others caring for patients with a sensory impairment
- Include community resources available for patients and families with a sensory impairment
- Include adaptations to the environment to maintain safety for the patient with a sensory impairment
- Incorporate nursing strategies to maximize sensory perception
- Outline nursing interventions for specific sensory disorders
- Identify evidence-based practices
Our five basic senses of sight (vision), hearing (auditory), touch (tactile), smell (olfactory), and taste (gustatory) help us perceive and act in the world around us. See Figure 7.1[13] for an illustration of our five senses.
We may not often consider the importance of our sensory input. As nurses, we especially rely on our senses when providing patient care as we gather assessment data. We ask questions and listen to patient responses, we listen to their heart and lung sounds, we evaluate the appearance of their skin, we may smell an infectious process when changing a wound dressing, and we feel the sensation of pulses when assessing circulation.
When an individual experiences sensory impairment because of the loss of one or more senses or is affected by the amount of stimuli (too much or too little), their ability to safely function is impacted. Nurses identify patients’ sensory impairments and implement interventions to improve their safety, functioning, and quality of life. The nurse’s goal is to provide support and dignity to individuals and their families by using strategies and resources that will help them to engage with their surroundings and others to the best of their ability.
This chapter will review common sensory impairments and related nursing care.
Interpreting Sensations
Before learning about sensory function, it is important to understand how the nervous system works. An intact nervous system is necessary for information to be delivered from the environment to the brain to trigger responses from the body. For neurons to transmit these messages, they are in the form of an action potential. Sensory receptors perceive a stimulus and then change the sensation to an electrical signal so that it can be transmitted to the brain and then out to the body. For example, a pain receptor perceives pain as your hand touches a hot tray. The signal is transmitted to the brain where it is interpreted, and then signals are quickly sent to the hand to pull away from the hot stimuli.[14]
Our bodies interpret sensations through a process using reception, perception, and reaction. Reception is the first part of the sensory process when a nerve cell or sensory receptor is stimulated by a sensation. Sensory receptors are activated by mechanical, chemical, or temperature stimuli. In addition to our five senses, we also have somatosensation. Somatosensation refers to sensory receptors that respond to stimuli such as pain, pressure, temperature, and vibration. It also includes vestibular sensation, a sense of spatial orientation and balance, and proprioception, the sense of the position of our bones, joints, and muscles. Although these sensory systems are all very different, they share a common purpose. They change a stimulus into an electrical signal that is transmitted in the nervous system.[15]
The sensory receptors for each of our senses work differently from one another. Light receptors, sound receptors, and touch receptors are each activated by different stimuli with specialized receptor specificity. For example, touch receptors are sensitive to pressure but do not have sensitivity to sound or light. Nerve impulses from sensory receptors travel along pathways to the spinal cord or directly to the brain. Some stimuli are also combined in the brain, such as our sense of smell that can affect our sense of taste.[16]
As an individual becomes aware of a stimulus and it is transmitted to the brain, perception occurs. Perception is the interpretation of a sensation. All sensory signals, except olfactory system input, are transmitted to the thalamus and to the appropriate region of the cortex of the brain. The thalamus, which is in the forebrain, acts as a relay station for sensory and motor signals. When a sensory signal leaves the thalamus, it is sent to the specific area of the cortex that processes that sense.[17] However, conditions that affect a person’s consciousness also affect the ability to perceive and interpret stimuli.
Reaction is the response that individuals have to a perception of a received stimulus. The brain determines what sensations are significant because it is impossible to react to all stimuli that are constantly received from our environment. A healthy brain maintains a balance between sensory stimuli received and those reaching awareness. However, sensory overload can occur if the amount of stimuli the brain is receiving is overwhelming to an individual. Sensory deprivation can also occur if there are insufficient sensations from the environment.[18]
Sensory Impairment
Alterations in sensory function include sensory impairment, sensory overload, and sensory deprivation. Sensory impairment includes any type of difficulty that an individual has with one of their five senses. When an individual experiences loss of a sensory function, such as vision, the way they interact with the environment is affected. For example, when an individual gradually loses their vision, their reliance on other senses to receive information from the environment is often enhanced.
Safety is always a nursing consideration for a patient with a sensory impairment. Intact senses are required to make decisions about functioning safely within the environment. For example, an individual who has impaired hearing may not be able to hear a smoke alarm and requires visual indicators when the alarm is triggered.
Sensory impairments are very common in older adults. Most older adults develop impaired near vision called presbyopia. See Figure 7.2[19] for an image of simulated presbyopia.
Deficits in taste and smell are also prevalent in this age group. Additionally, kinesthetic impairment (an altered sense of touch) can occur in adults as young as 55. Kinesthetic impairment can cause difficulty in daily functioning, such as buttoning one’s shirt or performing other fine motor tasks. These sensory losses can greatly impact how older adults live and function.[20]
Vision Impairments
Several types of visual impairments commonly occur in older adults, including macular degeneration, cataracts, glaucoma, diabetic retinopathy, and presbyopia. See Table 7.2 for more information about each of these visual conditions.
Table 7.2 Common Visual Conditions
| Macular Degeneration | Macular degeneration is the leading cause of legal blindness in individuals over 60 years of age. Risk factors include advancing age, a positive family history, hypertension, and smoking. In macular degeneration, there is loss of central vision with classic symptoms such as blurred central vision, distorted vision that causes difficulty driving and reading, and the requirement for brighter lights and magnification for close-up visual activities.[21] |
|---|---|
| Cataracts | Cataracts are the opacity of the lens of the eye that causes clouded, blurred, or dimmed vision. About half of individuals ages 65 to 75 will develop cataracts, with further incidence occurring after age 75. Cataracts can be removed with surgery that replaces the lens with an artificial lens.[22] |
| Glaucoma | Glaucoma is caused by elevated intraocular pressure that leads to progressive damage to the optic nerve, resulting in gradual loss of peripheral vision. It affects about 4% of individuals over age 70.[23] |
| Diabetic Retinopathy | Diabetic retinopathy is the leading cause of blindness in adults diagnosed with type 1 and type 2 diabetes mellitus. Diabetic retinopathy is a complication of diabetes mellitus due to damaged blood vessels in the retina causing vision loss.[24] Patients with diabetes are encouraged to receive annual eye exams so that retinopathy can be discovered and treated early. Treatments, such as laser treatment that can help shrink blood vessels, injections that can reduce swelling, or surgery, can prevent permanent vision loss.[25] |
| Presbyopia | As a person ages, the lens of the eye gradually becomes thicker and loses flexibility. It stops focusing light on the retina correctly, causing impaired near vision and accommodation at all distances. Presbyopia starts in the early to mid-forties and worsens with aging. It can lead to significant visual impairment but does not usually cause blindness.[26] |
Hearing Loss and Ear Problems
Approximately one third of individuals aged 70 and older have hearing loss. Good hearing depends on a series of events that change sound waves in the air into electrical signals. The auditory nerve conducts these electrical signals from the ear to the brain through a series of steps. The structures of the ear, such as the tympanic membrane and cochlea, must be intact and functioning appropriately for conduction of sound to occur. Age-related hearing loss (presbycusis) gradually occurs in most individuals as they age.[27] Typically, low-pitched sounds are easiest to hear, but it often becomes increasingly difficult to hear normal conversation, especially over loud background noise. Hearing aids are commonly used to enhance hearing. See Figure 7.3[28] for an image of common hearing aids used to treat hearing loss.

Hearing loss can be caused by other factors in addition to aging. A build-up of ear wax in the ear canal can cause temporary hearing loss. Sounds that are too loud or long-term exposure to loud noises can cause noise-induced hearing loss. For example, a loud explosion or employment using loud machinery without ear protection can damage the sensory hair cells in the ear. After these hair cells are damaged, the ability to hear is permanently diminished. Tinnitus, a medical term for ringing in the ears, can also occur. Some medications, such as high doses of aspirin or loop diuretics, can cause toxic effects to the sensory cells in the ear and lead to hearing loss or tinnitus.[29],[30] In addition to hearing loss, ear problems can also cause problems with balance, dizziness, and vertigo due to vestibular dysfunction.
Kinesthetic Impairments
Kinesthetic impairments, such as peripheral neuropathy, affect the ability to feel sensations. Symptoms of peripheral neuropathy include sensations of pain, burning, tingling, and numbness in the extremities that decrease a person’s ability to feel touch, pressure, and vibration. Position sense can also be affected and makes it difficult to coordinate complex movements, such as walking, fastening buttons, or maintaining balance when one’s eyes are closed. Peripheral neuropathy is caused by nerve damage that commonly occurs in patients with diabetes mellitus or peripheral vascular disease. It can also be caused by physical injuries, infections, autoimmune diseases, vitamin deficiencies, kidney diseases, liver diseases, and some medications.[31]
Life Span Considerations
Impaired sensory functioning increases the risk for social isolation in older adults. For example, when individuals are not able to hear well, they may pretend to hear in an attempt to avoid embarrassment when asking for the information to be repeated. They may begin to avoid noisy environments or stop participating socially in conversations around them.
Infants and children are also at risk for vision and hearing impairments related to genetic or prenatal conditions. Early determination of sensory impairments is crucial so that problems can be addressed with accommodations to minimize the impact on a child’s development. For example, a screening hearing test is completed on all newborns before discharge to evaluate for hearing impairments that can affect their speech development.
Sensory Overload and Sensory Deprivation
Stimuli are continually received from a variety of sources in our environment and from within our bodies. When an individual receives too many stimuli or cannot selectively filter out meaningful stimuli, sensory overload can occur. Symptoms of sensory overload include irritability, restlessness, covering ears or eyes to shield them from sensory input, and increased sensitivity to tactile input (i.e., scratchy fabric or sensations of medical equipment).[32] Sensory overload affects an individual’s ability to interpret stimuli from their environment and can lead to confusion and agitation. See Figure 7.4[33] of an image of a patient reacting to sensory overload.
The health care environment with its frequent noisy alarms, treatments, staff interruptions, and noisy hallway conversations can cause sensory overload for patients. Individuals have different tolerances for the amount of stimuli that will affect them adversely. Tolerance to stimuli is impacted by factors such as pain, stress levels, sleep patterns, physical health, and emotional health. When sensory overload occurs in a hospitalized patient, it can lead to delirium and acute confusion. It is important for the nurse to limit unnecessary awakenings and interactions with the health care team members when a patient is experiencing sensory overload.

Conversely, symptoms of sensory deprivation may occur when there are a lack of stimuli. People experiencing sensory deprivation often report perceptual disturbances such as hallucinations. Symptoms of sensory deprivation can mimic delirium, so it is important for a nurse to further investigate new perceptual disturbances.[34]

