5.7 Restraints
Definition of Restraints
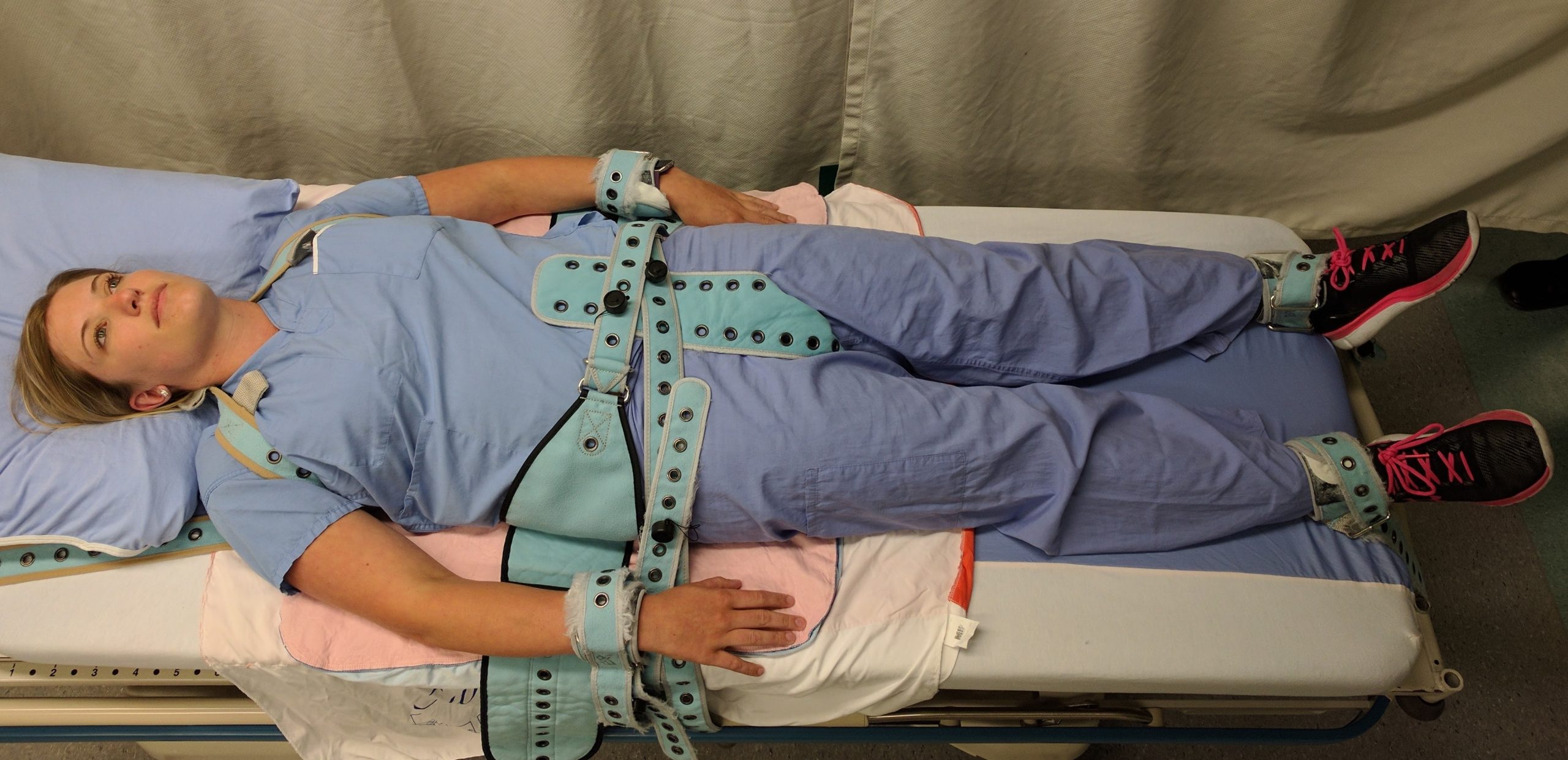
Restraints are devices used in health care settings to prevent patients from causing harm to themselves or others when alternative interventions are not effective. A restraint is a device, method, or process that is used for the specific purpose of restricting a patient’s freedom of movement without the permission of the person. See Figure 5.6[1] for an image of a simulated patient with restraints applied.
Restraints include mechanical devices such as a tie wrist device, chemical restraints, or seclusion. The Joint Commission defines chemical restraint as a drug used to manage a patient’s behavior, restrict the patient’s freedom of movement, or impair the patient’s ability to appropriately interact with their surroundings that is not standard treatment or dosage for the patient’s condition. It is important to note that the definition states the medication “is not standard treatment or dosage for the patient’s condition.”[2] Seclusion is defined as the confinement of a patient in a locked room from which they cannot exit on their own. It is generally used as a method of discipline, convenience, or coercion. Seclusion limits freedom of movement because, although the patient is not mechanically restrained, they cannot leave the area.
Although restraints are used with the intention to keep a patient safe, they impact a patient’s psychological safety and dignity and can cause additional safety issues and death. A restrained person has a natural tendency to struggle and try to remove the restraint and can fall or become fatally entangled in the restraint. Furthermore, immobility that results from the use of restraints can cause pressure injuries, contractures, and muscle loss. Restraints take a large emotional toll on the patient’s self-esteem and may cause humiliation, fear, and anger.
Restraint Guidelines
The American Nurses Association (ANA) has established evidence-based guidelines that state a restraint-free environment is the standard of care. The ANA encourages the participation of nurses to reduce patient restraints and seclusion in all health care settings. Restraining or secluding patients is viewed as contrary to the goals and ethical traditions of nursing because it violates the fundamental patient rights of autonomy and dignity. However, the ANA also recognizes there are times when there is no viable option other than restraints to keep a patient safe, such as during an acute psychotic episode when patient and staff safety are in jeopardy due to aggression or assault. The ANA also states that restraints may be justified in some patients with severe dementia or delirium when they are at risk for serious injuries such as a hip fracture due to falling.
The ANA provides the following guidelines: “When restraint is necessary, documentation should be done by more than one witness. Once restrained, the patient should be treated with humane care that preserves human dignity. In those instances where restraint, seclusion, or therapeutic holding is determined to be clinically appropriate and adequately justified, registered nurses who possess the necessary knowledge and skills to effectively manage the situation must be actively involved in the assessment, implementation, and evaluation of the selected emergency measure, adhering to federal regulations and the standards of The Joint Commission (2009) regarding appropriate use of restraints and seclusion.”[3] Nursing documentation typically includes information such as patient behavior necessitating the restraint, alternatives to restraints that were attempted, the type of restraint used, the time it was applied, the location of the restraint, and patient education regarding the restraint.
Any health care facility that accepts Medicare and Medicaid reimbursement must follow federal guidelines for the use of restraints. These guidelines include the following:
- When a restraint is the only viable option, it must be discontinued at the earliest possible time.
- Orders for the use of seclusion or restraint can never be written as a standing order or PRN (as needed).
- The treating physician must be consulted as soon as possible if the restraint or seclusion is not ordered by the patient’s treating physician.
- A physician or licensed independent practitioner must see and evaluate the need for the restraint or seclusion within one hour after the initiation.
- After restraints have been applied, the nurse should follow agency policy for frequent monitoring and regularly changing the patient’s position to prevent complications. Nurses must also ensure the patient’s basic needs (i.e., hydration, nutrition, and toileting) are met. Some agencies require a 1:1 patient sitter when restraints are applied.[4]
- Each written order for a physical restraint or seclusion is limited to 4 hours for adults, 2 hours for children and adolescents ages 9 to 17, or 1 hour for patients under 9. The original order may only be renewed in accordance with these limits for up to a total of 24 hours. After the original order expires, a physician or licensed independent practitioner (if allowed under state law) must see and assess the patient before issuing a new order.[5]
Side Rails and Enclosed Beds
Side rails and enclosed beds may also be considered a restraint, depending on the purpose of the device. Recall the definition of a restraint as “a device, method, or process that is used for the specific purpose of restricting a patient’s freedom of movement or access to movement without the permission of the person.” If the purpose of raising the side rails is to prevent a patient from voluntarily getting out of bed or attempting to exit the bed, then use of the side rails would be considered a restraint. On the other hand, if the purpose of raising the side rails is to prevent the patient from inadvertently falling out of bed, then it is not considered a restraint. If a patient does not have the physical capacity to get out of bed, regardless if side rails are raised or not, then the use of side rails is not considered a restraint.[6]
Hand Mitts
A hand mitt is a large, soft glove that covers a confused patient’s hand to prevent them from inadvertently dislodging medical equipment. Hand mitts are considered a restraint by The Joint Commission if used under these circumstances:
- Are pinned or otherwise attached to the bed or bedding
- Are applied so tightly that the patient’s hands or finger are immobilized
- Are so bulky that the patient’s ability to use their hands is significantly reduced
- Cannot be easily removed intentionally by the patient in the same manner it was applied by staff, considering the patient’s physical condition and ability to accomplish the objective[7]
It is important for the nurse to be aware of current best practices and guidelines for restraint use because they are continuously changing. For example, meal trays on chairs were previously used in long-term care facilities to prevent residents from getting out of the chair and falling. However, by the definition of a restraint, this action is now considered a restraint and is no longer used. Instead, several alternative interventions to restraints are now being used.
Alternatives to Restraints
Many alternatives to using restraints in long-term care centers have been developed. Most interventions focus on the individualization of patient care and elimination of medications with side effects that cause aggression and the need for restraints. Common interventions used as alternatives to restraints include routine daily schedules, regular feeding times, easing the activities of daily living, and reducing pain.[8]
Diversionary techniques such as television, music, games, or looking out a window can also be used to help to calm a restless patient. Encouraging restless patients to spend time in a supervised area, such as a dining room, lounge, or near the nurses’ station, helps to prevent their desire to get up and move around. If these techniques are not successful, bed and chair alarms or the use of a sitter at the bedside are also considered alternatives to restraints.
- “PinelRestraint.jpg” by James Heilman, MD is licensed under CC BY-SA 4.0 ↵
- The Joint Commission. https://www.jointcommission.org/ ↵
- American Nurses Association. (2012). Position statement: Reduction of patient restraint and seclusion in health care settings. https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/reduction-of-patient-restraint-and-seclusion-in-health-care-settings/ ↵
- Moore, G. P., & Pfaff, J. A. (2022, January 12). Assessment and emergency management of the acutely agitated or violent adult. UpToDate. Retrieved February 23, 2022, from https://www.uptodate.com/contents/assessment-and-emergency-management-of-the-acutely-agitated-or-violent-adult?csi=49b96b98-3589-484d-9a71-5c7a88d4fb72&source=contentShare ↵
- HealthPartners. (n.d.). Patients’ bill of rights (federal). https://www.healthpartners.com/care/hospitals/regions/patient-guest-support/federal-rights/ ↵
- The Joint Commission. (2020, June 29). Restraint and seclusion - Enclosure beds, side rails, and mitts. https://www.jointcommission.org/standards/standard-faqs/critical-access-hospital/provision-of-care-treatment-and-services-pc/000001668/ ↵
- The Joint Commission. (2020, June 29). Restraint and seclusion - Enclosure beds, side rails, and mitts. https://www.jointcommission.org/standards/standard-faqs/critical-access-hospital/provision-of-care-treatment-and-services-pc/000001668/ ↵
- Raveesh, B. N., Gowda, G. S., & Gowda, M. (2019). Alternatives to use of restraint: A path toward humanistic care. Indian Journal of Psychiatry, 61(Suppl 4), S693–S697. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6482675/ ↵
A device, method, or process that is used for the specific purpose of restricting a patient’s freedom of movement without the permission of the person.
A drug used to manage a patient’s behavior, restrict the patient’s freedom of movement, or impair the patient’s ability to appropriately interact with their surroundings that is not a standard treatment or dosage for the patient’s condition.
The confinement of a patient in a locked room from which they cannot exit on their own. It is generally used as a method of discipline, convenience, or coercion.

