8.3 Applying the Nursing Process
Now that we have discussed various concepts related to oxygenation and hypoxia, we will explain how a nurse uses the nursing process to care for patients with alterations in oxygenation.
Assessment
When assessing a patient’s oxygenation status, there are several subjective and objective assessments to include.
Subjective Assessment
The primary symptom to assess when a patient is experiencing decreased oxygenation is their level of dyspnea, the medical term for the subjective feeling of shortness of breath or difficulty breathing. Patients can be asked to rate their dyspnea on a scale of 0-10, similar to using a pain rating scale.[1] The feeling of dyspnea can be very disabling for patients. There are many interventions that a nurse can implement to help improve the feeling of dyspnea and, thus, improve a patient’s overall quality of life.
It is also important to ask patients if they are experiencing a cough. If a cough is present, determine if sputum is present, and if so, the color and amount of sputum. Sputum is mucus and other secretions that are coughed up from the mouth. The body always produces mucus to keep the delicate tissues of the respiratory tract moist so small particles of foreign matter can be trapped and forced out, but when there is an infection in the lungs, an excess of mucus is produced. The body attempts to get rid of this excess by coughing it up as sputum. The color of a patient’s sputum can provide cues for underlying medical conditions. For example, sputum caused by a respiratory infection is often yellow or green and often referred to as purulent sputum.[2] See Figure 8.7[3] for an image of purulent sputum.

Patients should be asked if they are experiencing chest pain. Chest pain can occur with several types of respiratory and cardiac conditions, some which are emergent. If the patient reports chest pain, first determine if it is an emergency by asking questions such as:
- “Does it feel like something is sitting on your chest?”
- “Is the pain radiating into your jaw or arm?”
- “Do you feel short of breath, dizzy, or nauseated?”
If any of these symptoms are occurring, seek emergency medical assistance according to agency policy. If it is not a medical emergency, perform a focused assessment on the chest pain, including onset, location, duration, characteristics, alleviating or aggravating factors, radiation, and if any treatment has been used for the pain.[4]
Objective Assessment
Focused objective assessments for a patient experiencing decreased oxygenation include assessing airway, evaluating respiratory rate and heart rate, analyzing pulse oximetry readings, and auscultating lung sounds for adventitious sounds.
Signs of cyanosis or clubbing should be noted. Clubbing is the enlargement of the fingertips that occurs with chronic hypoxia such as in chronic obstructive pulmonary disease (COPD) or congenital deficits in pediatric patients. See Figure 8.8[5] for an image of clubbing.

Another sign of chronic hypoxia that often occurs in patients with chronic obstructive pulmonary disease (COPD) includes an increased anterior-posterior chest diameter, often referred to as a barrel chest. A barrel chest results from air trapping in the alveoli. See Figure 8.9[6] for an image of a barrel chest.

Diagnostic Tests and Lab Work
Diagnostic tests and lab work are based on the patient’s medical condition that is causing the decreased oxygenation. For example, patients with a productive cough may have a chest X-ray or sputum culture ordered, and patients experiencing respiratory distress often have arterial blood gas (ABG) tests performed.
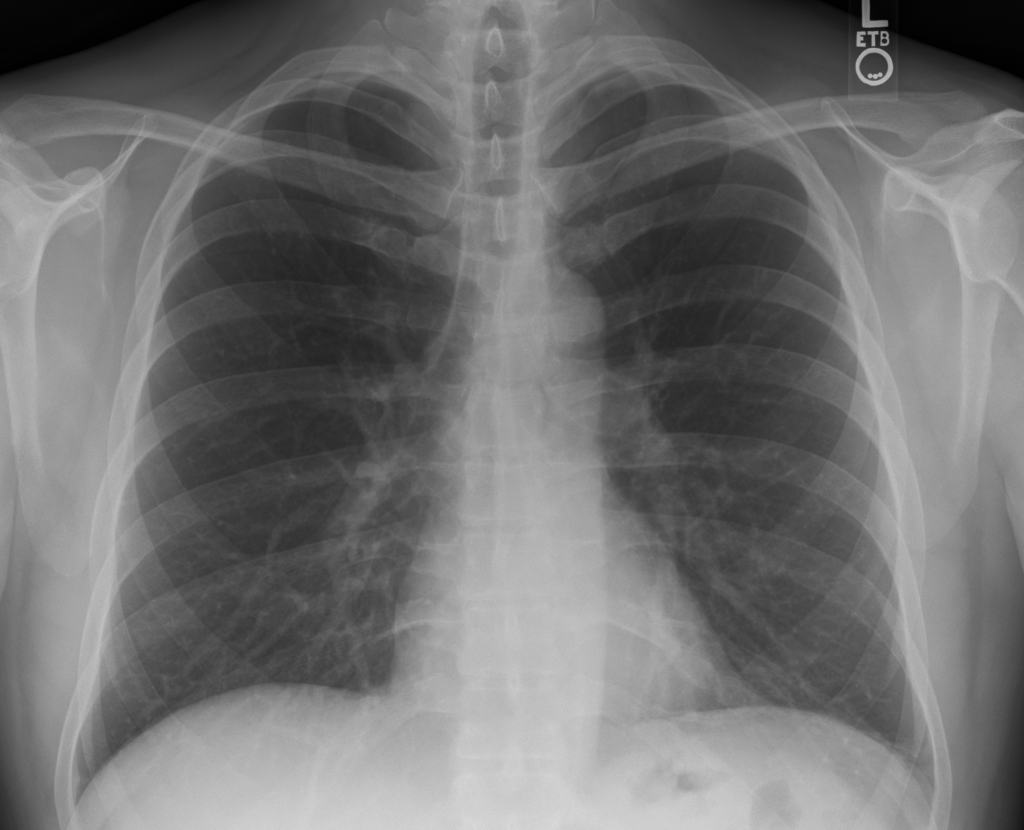
A chest X-ray is a fast and painless imaging test that uses certain electromagnetic waves to create pictures of the structures in and around the chest. This test can help diagnose and monitor conditions such as pneumonia, heart failure, lung cancer, and tuberculosis. Health care providers also use chest X-rays to see how well certain treatments are working and to check for complications after certain procedures or surgeries. Chest X-rays are contraindicated during pregnancy.[7],[8] See Figure 8.10[9] for an image of a chest X-ray.
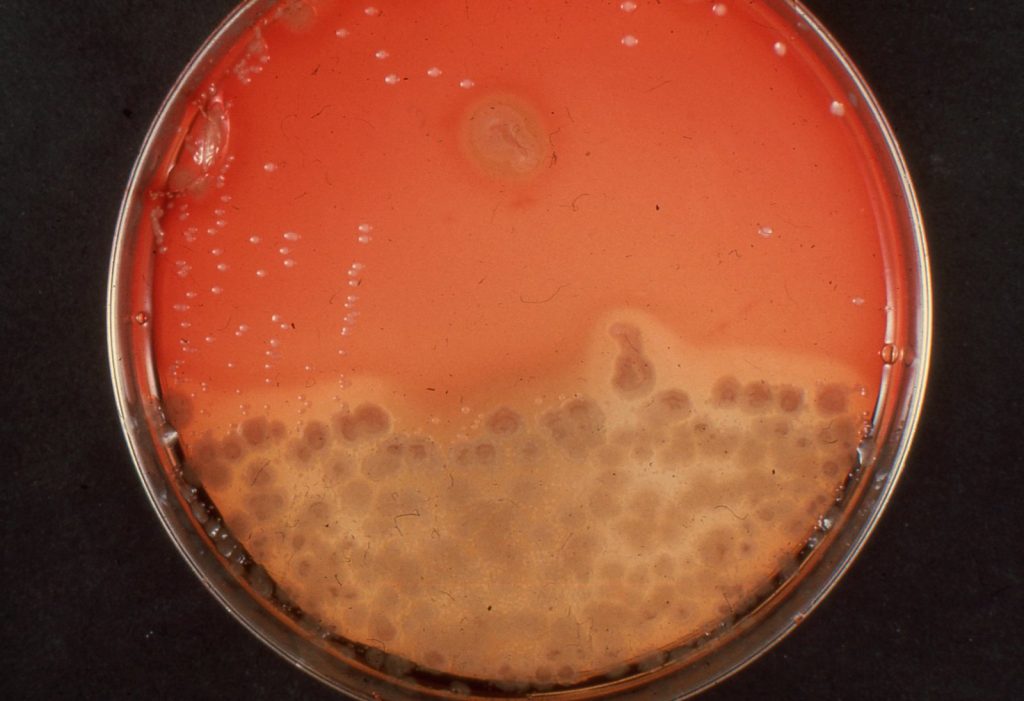
A sputum culture is a diagnostic test that evaluates the type and number of bacteria present in sputum. The patient is asked to cough deeply and spit any mucus that comes up into a sterile specimen container. The sample is sent to a lab where it is placed in a special dish and is watched for two to three days or longer to see if bacteria or other disease-causing germs grow.[10] See Figure 8.11[11] for an image of a sputum culture.
For patients experiencing respiratory distress, arterial blood gas (ABG) tests are often ordered. Additional details about ABG tests are discussed in the “Oxygenation Basic Concepts” section of this chapter, as well as in the “Acid-Base Balance” section of the “Fluid and Electrolytes” chapter. See Table 8.3a for a summary of normal ranges of ABG values in adults.
Table 8.3a Normal Ranges of ABG Values in Adults
| Value | Description | Normal Range |
|---|---|---|
| pH | Acid-base balance of blood | 7.35-7.45 |
| PaO2 | Partial pressure of oxygen | 80-100 mmHg |
| PaCO2 | Partial pressure of carbon dioxide | 35-45 mmHg |
| HCO3 | Bicarbonate level | 22-26 mEq/L |
| SaO2 | Calculated oxygen saturation | 95-100% |
Diagnoses
Commonly used NANDA-I nursing diagnoses for patients experiencing decreased oxygenation and dyspnea include Impaired Gas Exchange, Ineffective Breathing Pattern, Ineffective Airway Clearance, Decreased Cardiac Output, and Activity Intolerance. See Table 8.3b for definitions and selected defining characteristics for these commonly used nursing diagnoses.[12] Use a current, evidence-based nursing care plan resource when creating a care plan for a patient.
Table 8.3b NANDA-I Nursing Diagnoses Related to Decreased Oxygenation and Dyspnea
| NANDA-I Nursing Diagnoses | Definition | Selected Defining Characteristics |
|---|---|---|
| Impaired Gas Exchange | Excess or deficit in oxygenation and/or carbon dioxide elimination at the alveolar-capillary membrane. |
|
| Ineffective Breathing Pattern | Inspiration and/or expiration that does not provide adequate ventilation. | |
| Ineffective Airway Clearance | Inability to clear secretions or obstructions from the respiratory tract to maintain a clear airway. |
|
| Decreased Cardiac Output | Inadequate blood pumped by the heart to meet the metabolic demands of the body. |
|
| Activity Intolerance | Activity Intolerance: Insufficient physiological or psychological energy to endure or complete required or desired daily activities. |
|
For example, nurses commonly care for patients with chronic obstructive pulmonary disease (COPD). To select an accurate nursing diagnosis for a specific patient with COPD, the nurse compares findings obtained on patient assessment with the defining characteristics of various nursing diagnosis. The nurse selects Ineffective Breathing Pattern after validating this patient is demonstrating the associated signs and symptoms related to this nursing diagnosis:
-
- Dyspnea
- Increase in anterior-posterior chest diameter (e.g., barrel chest)
- Nasal flaring
- Orthopnea
- Prolonged expiration phase
- Pursed-lip breathing
- Tachypnea
- Use of accessory muscles to breathe
- Use of three-point position
Outcome Identification
A broad goal(s) for patients experiencing alterations in oxygenation is:
- The patient will have adequate movement of air into and out of the lungs.[13]
A sample “SMART” outcome criteria for a patient experiencing dyspnea is:
- The patient’s reported level of dyspnea will be within their stated desired range of 1-2 throughout their hospital stay.
Planning Interventions
According to NOC and NIC Linkages to NANDA-I and Clinical Conditions[14] and Nursing Interventions Classification (NIC),[15] Anxiety Reduction and Respiratory Monitoring are common categories of independent nursing interventions used to care for patients experiencing dyspnea and alterations in oxygenation. Anxiety Reduction is defined as, “Minimizing apprehension, dread, foreboding, or uneasiness related to an unidentified source of anticipated danger.”[16] Respiratory Monitoring is defined as, “Collection and analysis of patient data to ensure airway patency and adequate gas exchange.”[17] Selected nursing interventions related to anxiety reduction and respiratory monitoring are listed in the following box.
Selected Nursing Interventions to Reduce Anxiety and Perform Respiratory Monitoring
Anxiety Reduction
- Use a calm, reassuring approach
- Explain all procedures, including sensations likely to be experienced during the procedure
- Provide factual information concerning diagnosis, treatment, and prognosis
- Stay with the patient to promote safety and reduce fear
- Encourage the family to stay with the patient, as appropriate
- Listen attentively
- Create an atmosphere of trust
- Encourage verbalization of feelings, perceptions, and fears
- Identify when level of anxiety changes
- Provide diversional activities geared toward the reduction of tension
- Instruct the patient on the use of relaxation techniques
- Administer medications to reduce anxiety, as appropriate
Respiratory Monitoring
- Monitor rate, rhythm, depth, and effort of respirations
- Note chest movement, watching for symmetry and use of accessory muscles
- Monitor for noisy respirations such as snoring
- Monitor breathing patterns
- Monitor oxygen saturation levels in sedated patients
- Provide for noninvasive continuous oxygen sensors with appropriate alarm systems in patients with risk factors per agency policy and as indicated
- Auscultate lung sounds, noting areas of decreased or absent ventilation and presence of adventitious sounds
- Monitor patient’s ability to cough effectively
- Note onset, characteristics, and duration of cough
- Monitor the patient’s respiratory secretions
- Provide frequent intermittent monitoring of respiratory status in at-risk patients
- Monitor for dyspnea and events that improve and worsen it
- Monitor chest X-ray reports as appropriate
- Note changes in ABG values as appropriate
- Institute resuscitation efforts as needed
- Institute respiratory therapy treatments as needed
In addition to the independent nursing interventions listed in the preceding box, several nursing interventions can be implemented to manage hypoxia, such as teaching enhanced breathing and coughing techniques, repositioning, managing oxygen therapy, administering medications, and providing suctioning. Refer to Table 8.2b in the “Oxygenation Basic Concepts” section earlier in this chapter for information about these interventions.
For additional details regarding managing oxygen therapy, see the “Oxygen Therapy” chapter in Open RN Nursing Skills.
Read more information about respiratory medications in the “Respiratory” chapter in Open RN Nursing Pharmacology.
Patients should also receive individualized health promotion patient education to enhance their respiratory status. Health promotion education includes encouraging activities such as the following:
- Receiving an annual influenza vaccine
- Receiving a pneumococcal vaccine every five years as indicated
- Stopping smoking
- Drinking adequate fluids to thin respiratory secretions
- Participating in physical activity as tolerated
Implementing Interventions
When implementing interventions that have been planned to enhance oxygenation, it is always important to assess the patient’s current level of dyspnea and modify interventions based on the patient’s current status. For example, if dyspnea has worsened, some interventions may no longer be appropriate (such as ambulating), and additional interventions may be needed (such as consulting with a respiratory therapist or administering additional medication).
Evaluation
After implementing interventions, the effectiveness of interventions should be documented and the overall nursing care plan evaluated. Focused reassessments for evaluating improvement of oxygenation status include analyzing the patient’s heart rate, respiratory rate, pulse oximetry reading, and lung sounds, in addition to asking the patient to rate their level of dyspnea.
- Registered Nurses' Association of Ontario. (2005). Nursing care of dyspnea: The 6th vital sign in individuals with chronic obstructive pulmonary disease. https://rnao.ca/bpg/guidelines/dyspnea ↵
- Barrel, A. (2017, August 13). What is a sputum culture test? MedicalNewsToday. https://www.medicalnewstoday.com/articles/318924#what-is-a-sputum-culture-test ↵
- “Sputnum.JPG” by Zhangmoon618 is licensed under CC0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Chest Pain; [updated 2020, August 4]. https://medlineplus.gov/ency/article/003079.htm ↵
- “Acopaquia.jpg” by Desherinka is licensed under CC BY-SA 4.0 ↵
- “Normal A-P Chest Image.jpg" and "Barrel Chest.jpg" by Meredith Pomietlo for Chippewa Valley Technical College are licensed under CC BY 4.0 ↵
- National Heart, Lung, and Blood Institute. (n.d.) Chest x-ray. https://www.nhlbi.nih.gov/health-topics/chest-x-ray ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Chest x-ray; [updated 2020, August 4]. https://medlineplus.gov/ency/article/003804.htm ↵
- “Chest Xray PA 3-8-2010.png” by Stillwaterising is licensed under CC0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Routine sputum culture; [updated 2020, Aug 4]. https://medlineplus.gov/ency/article/003723.htm ↵
- “m241-8 Blood agar culture of sputum from patient with pneumonia. Comprimised host. Colonies of Candida albicans and pseudomonas aeruginosa (LeBeau)” by Microbe World is licensed under CC BY-NC-SA 2.0 ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York, p. 230. ↵
- Johnson, M., Moorhead, S., Bulechek, G., Butcher, H., Maas, M., & Swanson, E. (2012). NOC and NIC linkages to NANDA-I and clinical conditions: Supporting critical reasoning and quality care. Elsevier, pp. 54-55. ↵
- Johnson, M., Moorhead, S., Bulechek, G., Butcher, H., Maas, M., & Swanson, E. (2012). NOC and NIC linkages to NANDA-I and clinical conditions: Supporting critical reasoning and quality care. Elsevier, pp. 54-55 ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier, pp. 71 and 321 ↵
- Johnson, M., Moorhead, S., Bulechek, G., Butcher, H., Maas, M., & Swanson, E. (2012). NOC and NIC linkages to NANDA-I and clinical conditions: Supporting critical reasoning and quality care. Elsevier, pp. 54-55 ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier, pp. 71 and 321 ↵
Mucus and other secretions that are coughed up from the mouth.
Yellow or green sputum that often indicates a respiratory infection.
Enlargement of the fingertips that occurs with chronic hypoxia.
An increased anterior-posterior chest diameter, resulting from air trapping in the alveoli, that occurs in chronic respiratory disease.
Decreased respiratory rate less than the normal range according to the patient’s age.
Difficulty in breathing that occurs when lying down and is relieved upon changing to an upright position.
Elevated respiratory rate above normal range according to the patient’s age.

