9.3 Natural Defenses Against Infection
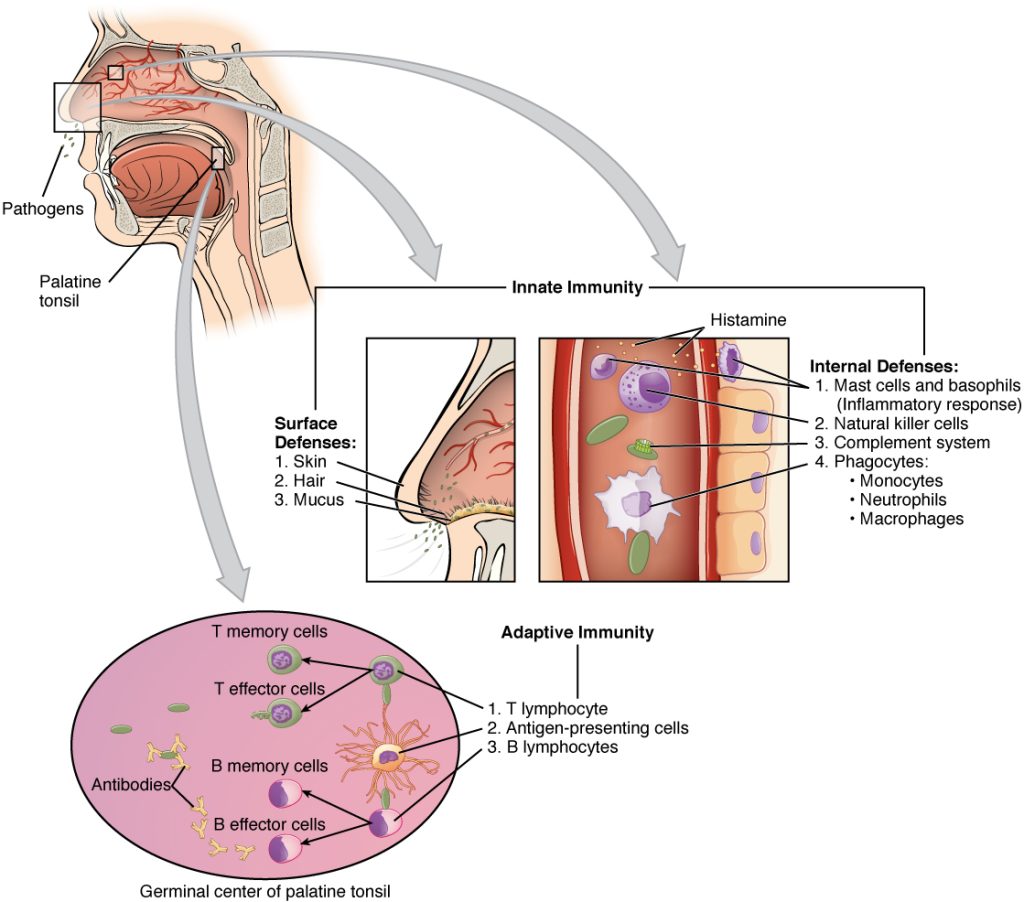
There are two basic ways the body defends against pathogens: nonspecific innate immunity and specific adaptive immunity.
Nonspecific Innate Immunity
Nonspecific innate immunity is a system of defenses in the body that targets invading pathogens in a nonspecific manner. It is called “innate” because it is present from the moment we are born. Nonspecific innate immunity includes physical defenses, chemical defenses, and cellular defenses.[1]
Physical Defenses
Physical defenses are the body’s most basic form of defense against infection. They include physical barriers to microbes, such as skin and mucous membranes, as well as mechanical defenses that physically remove microbes and debris from areas of the body where they might cause harm or infection. In addition, a person’s microbiome provides physical protection against disease as normal flora compete with pathogens for nutrients and cellular-binding sites.[2]
Skin
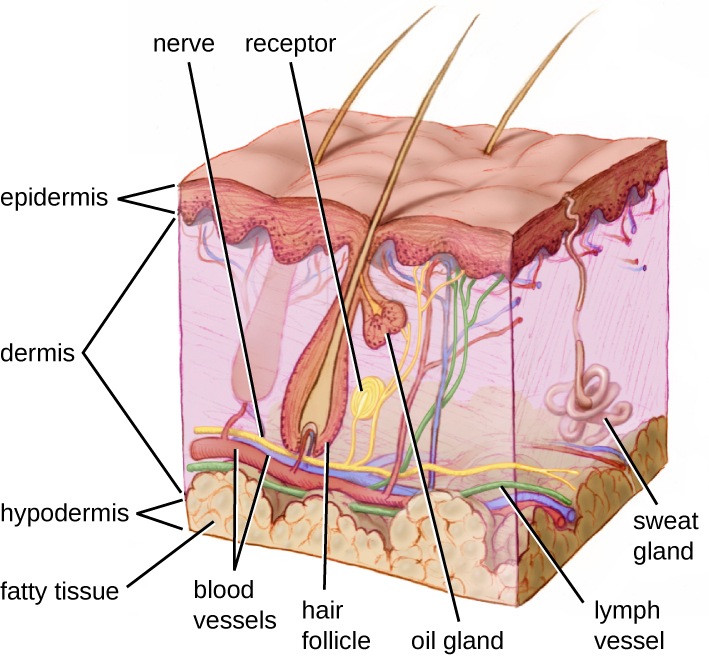
One of the body’s most important physical barriers is the skin barrier, which is composed of three layers of closely packed cells. See Figure 9.5[3] for an illustration of the layers of skin. The topmost layer of skin called the epidermis consists of cells that are packed with keratin. Keratin makes the skin’s surface mechanically tough and resistant to degradation by bacteria. Infections can occur when the skin barrier is broken, allowing the entry of opportunistic pathogens that infect the skin tissue surrounding the wound and possibly spread to deeper tissues.[4]
Mucus Membranes
The mucous membranes lining the nose, mouth, lungs, and urinary and digestive tracts provide another nonspecific barrier against potential pathogens. Mucous membranes consist of a layer of epithelial cells bound by tight junctions. The epithelial cells secrete a moist, sticky substance called mucous. Mucous covers and protects the fragile cell layers beneath it and also traps debris, including microbes. Mucus secretions also contain antimicrobial peptides.[5]
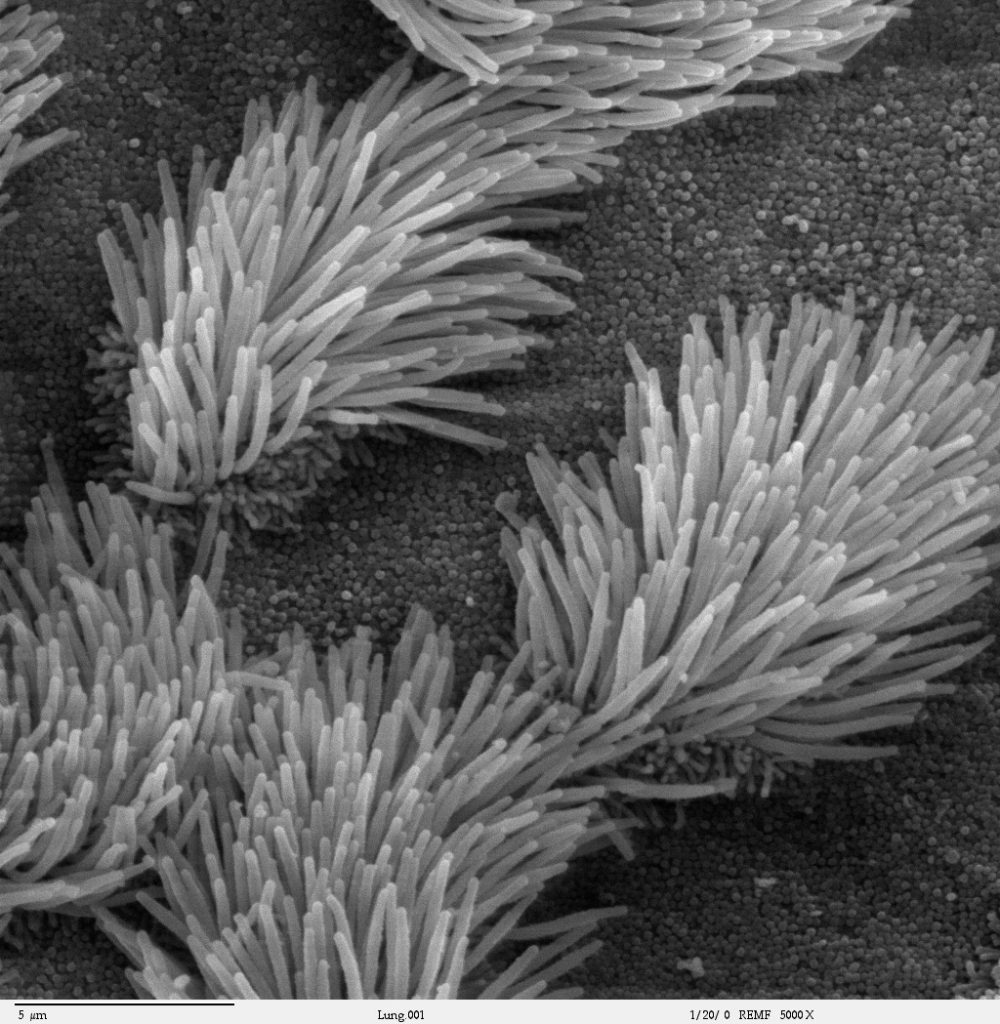
In many regions of the body, mechanical actions flush mucus (along with trapped or dead microbes) out of the body or away from potential sites of infection. For example, in the respiratory system, inhalation can bring microbes, dust, mold spores, and other small airborne debris into the body. This debris becomes trapped in the mucus lining the respiratory tract. The epithelial cells lining the upper parts of the respiratory tract have hair-like appendages known as cilia. Movement of the cilia propels debris-laden mucus out and away from the lungs. The expelled mucus is then swallowed and destroyed in the stomach, coughed up, or sneezed out. This system of removal is often called the mucociliary escalator. Disruption of the mucociliary escalator by the damaging effects of smoking can lead to increased colonization of bacteria in the lower respiratory tract and frequent infections, which highlights the importance of this physical barrier to host defenses.[6] See Figure 9.6[7] for an image of a magnified mucociliary escalator.
Like the respiratory tract, the digestive tract is a portal of entry through which microbes enter the body, and the mucous membranes lining the digestive tract provide a nonspecific physical barrier against ingested microbes. The intestinal tract is lined with epithelial cells, interspersed with mucus-secreting goblet cells. This mucus mixes with material received from the stomach, trapping foodborne microbes and debris, and the mechanical action of peristalsis (a series of muscular contractions in the digestive tract) moves this mixture through the intestines and excretes it in feces.[8] For this reason, feces can contain microorganisms that can cause the spread of infection; therefore, good hand hygiene is vital.
Endothelia
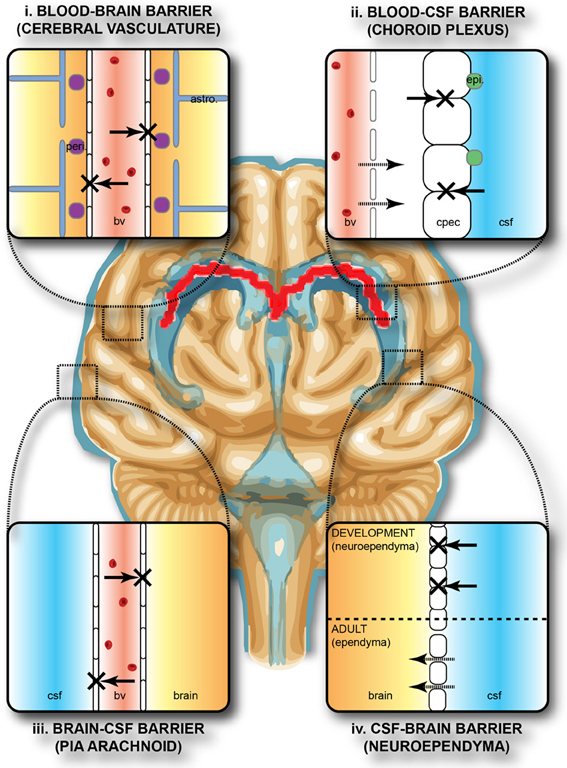
The epithelial cells lining the urogenital tract, blood vessels, lymphatic vessels, and other tissues are known as endothelia. These tightly packed cells provide an effective frontline barrier against invaders. The endothelia of the blood-brain barrier, for example, protects the central nervous system (CNS) from microorganisms. Infection of the CNS can quickly lead to serious and often fatal inflammation. The protection of the blood-brain barrier keeps the cerebrospinal fluid that surrounds the brain and spinal cord sterile.[9] See Figure 9.7[10] for an illustration of the blood-brain barrier.
Mechanical Defenses
In addition to physical barriers that keep microbes out, the body has several mechanical defenses that physically remove pathogens from the body and prevent them from taking up residence. For example, the flushing action of urine and tears serves to carry microbes away from the body. The flushing action of urine is responsible for the normally sterile environment of the urinary tract. The eyes have additional physical barriers and mechanical mechanisms for preventing infections. The eyelashes and eyelids prevent dust and airborne microorganisms from reaching the surface of the eye. Any microbes or debris that make it past these physical barriers are flushed out by the mechanical action of blinking, which bathes the eye in tears, washing debris away.[11] See Figure 9.8[12] for an image of an infant’s eyelashes that prevent dust from reaching the surface of the eye.

Microbiome
Normal flora that contribute to an individual’s microbiome serve as an important first-line defense against invading pathogens. Through their occupation of cellular binding sites and competition for available nutrients, normal flora prevent the early steps of pathogen attachment and proliferation required for the establishment of an infection. For example, in the vagina, normal flora compete with opportunistic pathogens like Candida albicans. This competition prevents yeast infection by limiting the availability of nutrients and inhibiting the growth of Candida, keeping its population in check. Similar competitions occur between normal flora and potential pathogens on the skin, in the upper respiratory tract, and in the gastrointestinal tract.[13]
The importance of the normal flora in host defenses is highlighted by a person’s increased susceptibility to infectious diseases when their microbiome is disrupted or eliminated. For example, treatment with antibiotics can significantly deplete the normal flora of the gastrointestinal tract, providing an advantage for pathogenic bacteria such as Clostridium difficile (C-diff) to colonize and cause diarrheal infection. Diarrhea caused by C-diff can be severe and potentially lethal. In fact, a recent strategy for treating recurrent C-diff infections is fecal transplantation that involves the transfer of fecal material from a donor into the intestines of the patient as a method of restoring their normal flora.[14]
Chemical Defenses
In addition to physical defenses, our nonspecific innate immune system uses several chemical mediators that inhibit microbial invaders. The term chemical mediators encompasses a wide array of substances found in various fluids and tissues throughout the body. For example, sebaceous glands in the dermis secrete an oil called sebum that is released onto the skin surface through hair follicles. Sebum provides an additional layer of defense by helping seal off the pore of the hair follicle and preventing bacteria on the skin’s surface from invading sweat glands and surrounding tissue. Environmental factors can affect these chemical defenses of the skin. For example, low humidity in the winter makes the skin more dry and susceptible to pathogens normally inhibited by the skin’s low pH. Application of skin moisturizer restores moisture and essential oils to the skin and helps prevent dry skin from becoming infected.[15]
Examples of other chemical defenses are enzymes, pH level, and chemical mediators. Enzymes in saliva and the digestive tract eliminate most pathogens that manage to survive the acidic environment of the stomach. In the urinary tract, the slight acidity of urine inhibits the growth of potential pathogens in the urinary tract. The respiratory tract also uses various chemical mediators in the nasal passages, trachea, and lungs that have antibacterial properties.[16]
Plasma Protein Mediators
In addition to physical, mechanical, and chemical defenses, there are also nonspecific innate immune factors in plasma, the fluid portion of blood, such as acute-phase proteins, complement proteins, and cytokines. These plasma protein mediators contribute to the inflammatory response.[17]
An example of an acute-phase protein is C-reactive protein. High levels of C-reactive protein indicate a serious infection or other medical condition that causes inflammation is occurring.[18]
Complement proteins are always present in the blood and tissue fluids, allowing them to be activated quickly. They aid in the destruction of pathogens by piercing their outer membranes (cell lysis) or by making them more attractive to phagocytic cells such as macrophages.[19]
Cytokines are proteins that affect interaction and communication between cells. When a pathogen enters the body, the first immune cell to notice the pathogen is like the conductor of an orchestra. That cell directs all the other immune cells by creating and sending out messages (cytokines) to the rest of the organs or cells in the body to respond to and initiate inflammation. Too many cytokines can have a negative effect and result in what’s known as a cytokine storm.[20],[21] A cytokine storm is a severe immune reaction in which the body releases too many cytokines into the blood too quickly. A cytokine storm can occur as a result of an infection, autoimmune condition, or other disease. Signs and symptoms include high fever, inflammation, severe fatigue, and nausea. A cytokine storm can be severe or life-threatening and lead to multiple organ failure. For example, many COVID-19 complications and deaths were caused by a cytokine storm.[22],[23]
Inflammation
Inflammation is a response triggered by a cascade of chemical mediators and occurs when pathogens successfully breach the nonspecific innate immune system or when an injury occurs. Although inflammation is often perceived as a negative consequence of injury or disease, it is a necessary process that recruits cellular defenses needed to eliminate pathogens, remove damaged and dead cells, and initiate repair mechanisms. Excessive inflammation, however, can result in local tissue damage, and in severe cases, such as sepsis, it can become deadly.[24]
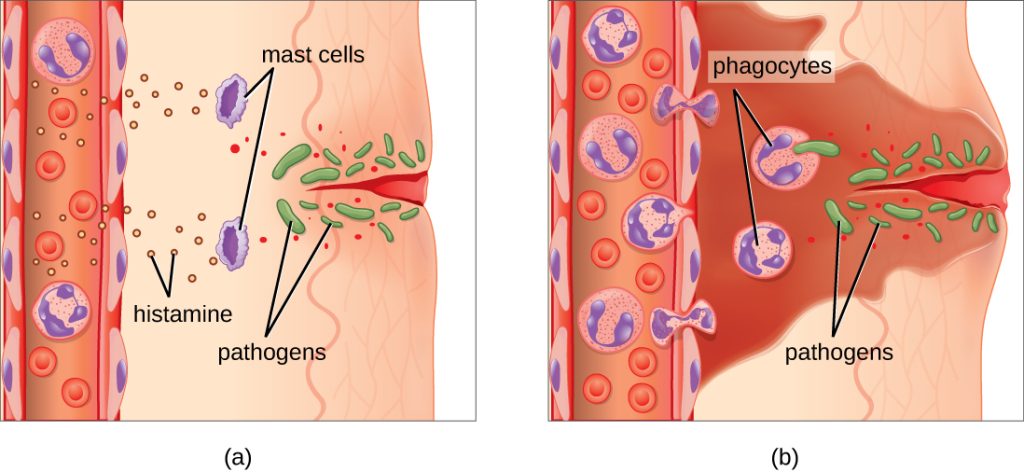
An immediate response to tissue injury is acute inflammation. Vasoconstriction occurs to minimize blood loss if injury has occurred. Vasoconstriction is followed by vasodilation with increased permeability of the blood vessels due to the release of histamine by mast cells. Histamine contributes to the five observable signs of the inflammatory response: erythema (redness), edema (swelling), heat, pain, and altered function. It is also associated with an influx of phagocytes at the site of injury and/or infection. See Figure 9.9[25] for an illustration of the inflammatory response, with (a) demonstrating when mast cells detect injury to nearby cells and release histamine, initiating an inflammatory response and (b) illustrating where histamine increases blood flow to the wound site and the associated increased vascular permeability allows fluid, proteins, phagocytes, and other immune cells to enter infected tissue. These events result in the swelling and reddening of the injured site. The increased blood flow to the injured site causes it to feel warm. Inflammation is also associated with pain due to these events stimulating nerve pain receptors in the tissue. Increasing numbers of neutrophils are then recruited to the area to fight pathogens. As the fight rages on, white blood cells are recruited to the area, and pus forms from the accumulation of neutrophils, dead cells, tissue fluids, and lymph. Typically, after a few days, macrophages clear out this pus.[26] During injury, if this nonspecific inflammatory process does not successfully kill the pathogens, infection occurs.
Fever
A fever is part of the inflammatory response that extends beyond the site of infection and affects the entire body, resulting in an overall increase in body temperature. Like other forms of inflammation, a fever enhances the nonspecific innate immune defenses by stimulating white blood cells to kill pathogens. The rise in body temperature also inhibits the growth of many pathogens. During fever, the patient’s skin may appear pale due to vasoconstriction of the blood vessels in the skin to divert blood flow away from extremities, minimize the loss of heat, and raise the body’s core temperature. The hypothalamus also stimulates the shivering of muscles to generate heat and raise the core temperature.[27]
A low-level fever is thought to help an individual overcome an illness. However, in some instances, this immune response can be too strong, causing tissue and organ damage and, in severe cases, even death. For example, Staphylococcus aureus and Streptococcus pyogenes are capable of producing superantigens that cause toxic shock syndrome and scarlet fever, respectively. Both of these conditions are associated with extremely high fevers in excess of 42 °C (108 °F) that must be managed to prevent tissue injury and death.[28]
When a fever breaks, the hypothalamus stimulates vasodilation, resulting in a return of blood flow to the skin and a subsequent release of heat from the body. The hypothalamus also stimulates sweating, which cools the skin as the sweat evaporates.[29]
Specific Adaptive Immunity
Now that we have discussed several nonspecific innate defenses against a pathogen, let’s discuss specific adaptive immunity. Specific adaptive immunity is the immune response that is activated when the nonspecific innate immune response is insufficient to control an infection. There are two types of adaptive responses: the cell-mediated immune response, which is carried out by T cells, and the humoral immune response, which is controlled by activated B cells and antibodies.[30]
B cells mature in the bone marrow. B cells make Y-shaped proteins called antibodies that are specific to each pathogen and lock onto its surface and mark it for destruction by other immune cells. The five classes of antibodies are IgG, IgM, IgA, IgD, and IgE. They also turn into memory B cells.[31]
T cells mature in the thymus. T cells are categorized into three classes: helper T cells, regulatory T cells, and cytotoxic T cells. Helper T cells stimulate B cells to make antibodies and help killer cells develop. Killer T cells directly kill cells that have already been infected by a pathogen. T cells also use cytokines as messenger molecules to send chemical instructions to the rest of the immune system to ramp up its response.[32]
Specific adaptive immunity also creates memory cells for each specific pathogen that provides the host with long-term protection from reinfection with that pathogen. On reexposure, these memory cells facilitate an efficient and quick immune response. For example, when an individual recovers from chicken pox, the body develops a memory of the varicella-zoster virus that will specifically protect it from reinfection if it is exposed to the virus again.[33]
See Figure 9.10[34] for an illustration of innate immunity and specific adaptive immunity that occurs in response to a pathogen entering the body through the nose.
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “OSC_Microbio_17_02_Skin.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology@9.8/pages/17-1-physical-defenses. ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- The Integrative HMP (iHMP) Research Network Consortium. (2019). Proctor, L. M., Creasy, H. H., et. al. The integrative human microbiome project. Nature, 569, 641–648. https://doi.org/10.1038/s41586-019-1238-8 ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “Bronchiolar_epithelium_3_-_SEM.jpg” by Charles Daghlian is licensed by CC0 ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “Protective_barriers_of_the_brain.jpg” by Stolp H. B., Liddelow S. A., Sá-Pereira I., Dziegielewska K. M., & Saunders N. R. is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “Eyelashes_of_a_2-month-old_baby_boy.png” by Karthik.yerramilly is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Concepts of Biology - 1st Canadian Edition by Molnar & Gair and is licensed under CC BY 4.0. ↵
- Sproston, N. R., & Ashworth, J. J. (2018). Role of c-reactive protein at sites of inflammation and infection. Frontiers in Immunology, 9, 754. https://doi.org/10.3389/fimmu.2018.00754 ↵
- Complement. (2018). In Britannica. https://www.britannica.com/science/complement-immune-system-component ↵
- Arango Duque, G., & Descoteaux, A. (2014). Macrophage cytokines: Involvement in immunity and infectious diseases. Frontiers in Immunology, 5, 491. https://doi.org/10.3389/fimmu.2014.00491 ↵
- National Cancer Institute (n.d.) NCI Dictionary of Cancer Terms. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cytokine-storm ↵
- Hojyo, S., Uchida, M., Tanaka, K., et al. (2020). How COVID-19 induces cytokine storm with high mortality. Inflammation and Regeneration, 40(37). https://doi.org/10.1186/s41232-020-00146-3 ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “OSC_Microbio_17_06_Erythema.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology@9.8/pages/17-5-inflammation-and-fever. ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “2211_Cooperation_Between_Innate_and_Immune_Responses.jpg” by OpenStax is licensed under CC BY 3.0. ↵
A system of defenses in the body that targets invading pathogens in a nonspecific manner that is present from the moment we are born.
The involuntary contraction and relaxation of the muscles of the intestine creating wave-like movements that push the digested contents forward.
Proteins that affect interaction and communication between cells.
Severe immune reaction in which the body releases too many cytokines into the blood too quickly.
A response triggered by a cascade of chemical mediators that occur when pathogens successfully breach the nonspecific physical defenses of the immune system or when an injury occurs.
Immune cells that mature in the bone marrow and produce antibodies.
Y proteins created by B cells that are specific to each pathogen and lock onto its surface and mark it for destruction by other immune cells.
Immune cells that mature in the thymus.
The immune response that is activated when the nonspecific innate immune response is insufficient to control an infection.

