23.4 IV Therapy Site Assessment & Complications
Catheter Size and Type Selection
Peripheral IV catheters are available in a variety of sizes, most commonly ranging from 14 gauge to 26 gauge. Note that the lower the gauge size, the wider the diameter of the catheter, with 14-gauge catheters allowing for the greatest flow rate.[1] Catheter sizes are color coded to allow for easy identification of the catheter size after a vein is accessed. See Figure 23.12[2] for colors associated with IV catheter sizes and their associated flow rates.
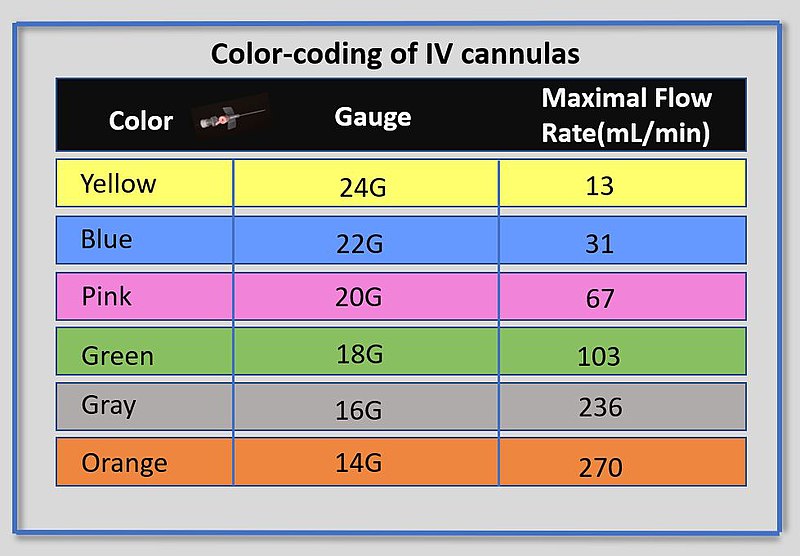
Nurses must consider the purpose for venous access, along with assessment of the patient’s vessel size, when selecting an IV catheter to attempt cannulation. The smallest IV catheter should be selected that will accommodate the prescribed therapy and patient need.[3]
Catheters with a smaller gauge (i.e., larger diameter) permit infusion of viscous fluids, such as blood products, at a faster rate with decreased opportunity for catheter occlusion.[4] Additionally, an appropriately sized catheter also allows for adequate blood flow around the catheter itself. The most common IV catheter size for adult patients is 18- or 20-gauge catheters. However, frail elderly patients and children have smaller vasculature, so a 22-gauge catheter is often preferred.
There are different manufacturer brands of IV catheters, but all include a beveled hollow needle, a flashback chamber in which blood can be visualized when entering the vein, and a flexible catheter that is left in the vein after the catheter has been threaded into the vein and the needle removed.
IV insertion equipment varies among institutions, but common types include shielded IV catheters or winged (i.e., “butterfly”) devices. Variation is often related to the presence of a stabilizing device at the site of insertion, as well as the presence of short extension tubing. For shielded catheter types, the stabilizing device and extension tubing are typically added to the catheter itself and not included with the cannulation needle. See Figure 23.13[5] for an image of shielded IV catheters.

Nurses must ensure the selected size and type of IV catheter are appropriate for the procedure or infusion that is ordered because not all peripheral IV catheters are suitable for all procedures. For example, if a procedure requires the infusion of contrast dye, a specific size infusion port is required.
Despite the wide variation in catheter equipment that is available, there has been significant focus among manufacturers regarding the need for safety equipment during venipuncture. Many devices utilize mechanisms to self-contain needles within a plastic sheath after withdrawal from the patient. These devices can be activated through a button in the devices or a manual trigger initiated by the individual attempting cannulation. Regardless of the type of safety lock, it is important to utilize the equipment as intended and never attempt to disable or override the mechanism. These mechanisms are important to help prevent accidental needlesticks or injury with a contaminated needle after it has been removed from the patient. Additionally, after cannulation is attempted, the individual who attempted cannulation is responsible for ensuring all needles are disposed of in a sharps container. It is good practice to be aware of how many sharps were brought into the room, opened, and disposed. This helps to ensure that any needles are not inadvertently left in a patient’s bed, tray table, floor, etc. Nurses must be familiar with the equipment used at the health care facility and receive orientation on the specific mechanics related to the equipment and safety practices.
Initiating Peripheral IV Access
The steps for initiating peripheral IV access are described in the Open RN Nursing Advanced Skills “Perform IV Insertion and IV Removal” checklist in Chapter 1.
Monitoring for Potential Complications
Several potential complications may arise from peripheral intravenous therapy. It is the responsibility of the nurse to prevent, assess, and manage signs and symptoms of complications. Complications can be categorized as local or systemic. See Table 23.4a for potential local complications of peripheral IV therapy.
Table 23.4a Local Complications of Peripheral IV Therapy[6],[7]
| Complications | Potential Causes and Prevention | Treatment |
|---|---|---|
| Phlebitis: The inflammation of the vein’s inner lining, the tunica intima. Clinical indications are localized redness, pain, heat, purulent drainage, and swelling that can track up the vein leading to a palpable venous cord. | Mechanical causes: Inflammation of the vein’s inner lining can be caused by the cannula rubbing and irritating the vein. To prevent mechanical inflammation, choose the smallest outer diameter of a catheter for therapy, secure the catheter with securement technology, avoid areas of flexion, and stabilize the joint as needed.[8]
Chemical causes: Inflammation of the vein’s inner lining can be caused by medications or fluids with high alkaline, acidic, or hypertonic qualities. To avoid chemical phlebitis, follow the parenteral drug therapy guidelines in a drug reference resource for administering IV medications, including the appropriate amount of solution and rate of infusion. Infectious causes: May be related to emergent VAD insertions, poor aseptic technique, or contaminated dressings. |
Chemical phlebitis: Evaluate infusion therapy and the need for different vascular access, different medication, slower rate of infusion, or more dilute infusate. If indicated, remove the Vascular Access Device (VAD).[9]
Transient mechanical phlebitis: May be treatable by stabilizing the catheter, applying heat, elevating limb, and providing analgesics as needed. Consider requesting other pharmacologic interventions such as anti-inflammatory agents if needed. Monitor site for 24 hours post-insertion, and if signs and symptoms persist, remove the catheter.[10] Infectious phlebitis: If purulent drainage is present or infection is suspected, remove the catheter and obtain a culture of the purulent drainage and catheter tip. Monitor for signs of systemic infection.[11] |
| Infiltration: A condition that occurs when a nonvesicant solution is inadvertently administered into surrounding tissue. Signs and symptoms include pain, swelling, redness, the skin surrounding the insertion site is cool to touch, there is a change in the quality or flow of IV, the skin is tight around the IV site, IV fluid is leaking from IV site, or there are frequent alarms on the IV pump. | Infiltration is one of the most common complications in infusion therapy involving an IV catheter.[12] For this reason, the patency of an IV site must always be checked before administering IV push medications.
Infiltration can be caused by piercing the vein, excessive patient movement, a dislodged or incorrectly placed IV catheter, or too rapid infusion of fluids or medications into a fragile vein. Always secure a peripheral IV catheter with tape or a stabilization device to avoid accidental dislodgement. Avoid sites that are areas of flexion. |
Stop the infusion and remove the cannula. Follow agency policy related to infiltration. |
| Extravasation: A condition that occurs when vesicant (an irritating solution or medication) is administered and inadvertently leaks into surrounding tissue and causes damage. It is characterized by the same signs and symptoms as infiltration but also includes burning, stinging, redness, blistering, or necrosis of the tissue. | Extravasation has the same potential causes of infiltration but with worse consequences because of the effects of vesicants. Extravasation can result in severe tissue injury and necrosis. For this reason, known vesicant medications should be administered via central lines. | Stop the infusion. Detach all administration sets and aspirate from the catheter hub prior to removing the catheter to remove vesicant medication from the catheter lumen and as much as possible from the subcutaneous tissue.[13]
Follow agency policy regarding extravasation of specific medications. For example, toxic medications have a specific treatment plan. |
| Hemorrhage: Bleeding from the IV access site. | Bleeding occurs when the IV catheter becomes dislodged. | If dislodgement occurs, apply pressure with gauze to the site until the bleeding stops and then apply a sterile transparent dressing. |
| Local infection: Infection at the site is indicated by purulent drainage, typically two to three days after an IV site is started. | Local infection is often caused by nonadherence to aseptic technique during IV initiation or IV maintenance or the dressing becomes contaminated or non-intact over the access site. | Remove the cannula and clean the site using sterile technique. If infection is suspected, remove the catheter and obtain a culture of the purulent drainage and catheter tip. Monitor for signs of systemic infection. |
| Nerve injury[14] | Paresthesia-type pain occurring during venipuncture or during an indwelling IV catheter can indicate nerve injury. | Immediately remove the cannula, notify the provider, and document findings in the chart. |
In addition to local complications that can occur at the site of IV insertion, there are many systemic complications that nurses must monitor for when initiating peripheral IV access, as well as monitoring a patient receiving IV therapy. See Table 23.4b for a list of systemic complications, signs, symptoms, and treatment.
Table 23.4b Systemic Complications of Peripheral IV Therapy[15]
| Complication | Signs, Symptoms, and Treatment |
|---|---|
| Pulmonary Edema | Pulmonary edema, also known as fluid overload or circulatory overload, is a condition caused by excess fluid accumulation in the lungs due to excessive fluid in the circulatory system. It is characterized by decreased oxygen saturation; increased respiratory rate; fine or coarse crackles in the lung bases; restlessness; breathlessness; dyspnea; and coughing up pink, frothy sputum. Pulmonary edema requires prompt medical attention and treatment. If pulmonary edema is suspected, raise the head of the bed, apply oxygen, take vital signs, complete a cardiovascular assessment, and immediately notify the provider. |
| Air Embolism | An air embolism refers to the presence of air in the cardiovascular system. It occurs when air is introduced into the venous system and travels to the right ventricle and/or pulmonary circulation. Air embolisms can occur during catheter insertion, changing IV bags, adding secondary medication administration, and catheter removal. Inadvertent administration of 10 mL of air can have serious and fatal consequences. However, small air bubbles are tolerated by most patients. Signs and symptoms of an air embolism include sudden shortness of breath, continued coughing, breathlessness, shoulder or neck pain, agitation, feeling of impending doom, light-headedness, hypotension, wheezing, increased heart rate, altered mental status, and jugular venous distension.
If an air embolism is suspected, occlude the source of air entry. Place the patient in a Trendelenburg position on their left side (if not contraindicated), apply oxygen at 100%, obtain vital signs, and immediately notify the provider. To prevent air embolisms, perform the following steps when administering IV therapy: ensure the drip chamber is one-third to one-half filled, remove all air from the IV tubing by priming it prior to attaching it to the patient, use precautions when changing IV bags or adding secondary medication bags, ensure all IV connections are tight, and ensure clamps are used when the IV system is not in use. |
| Catheter Embolism | A catheter embolism occurs when a small part of the cannula breaks off and flows into the vascular system. When removing a peripheral IV cannula, inspect the catheter tip to ensure the end is intact. Notify the provider immediately if the catheter tip is not intact when it is removed. |
| Catheter-Related Bloodstream Infection (CR-BSI) | Catheter-related bloodstream infection (CR-BSI) is caused by microorganisms introduced into the bloodstream through the puncture site, the hub, or contaminated IV tubing or IV solution, leading to bacteremia or sepsis. A CR-BSI is a hospital-acquired preventable infection and considered an adverse event. A CR-BSI is diagnosed when infection occurs with one positive blood culture in a patient with a vascular device (or a patient who had a vascular device within 48 hours before the infection) with no apparent source for the infection other than the vascular access device. Treatment for CR-BSI is IV antibiotic therapy.
To prevent CR-BSI, it is vital to perform hand hygiene prior to care and maintenance of an IV system and to use strict aseptic technique for care and maintenance of all IV therapy procedures. |
- This work is a derivative of StatPearls by Beecham & Tackling and is licensed under CC BY 4.0 ↵
- “Color-coding_of_IV_cannulas.jpg” by Dr.Vijaya Chandar is licensed under CC BY-SA 4.0 ↵
- Gorski, L. A., Hadaway, L., Hagle, M. E., Broadhurst, D., Clare, S., Kleidon, T., Meyer, B. M., Nickel, B., Rowley, S., Sharp, E., & Alexander, M. A. (2021). Infusion therapy standards of practice. Journal of Infusion Nursing, 44(Suppl 1S), S1–S224. https://doi: 10.1097/NAN.0000000000000396.org ↵
- This work is a derivative of StatPearls by Beecham & Tackling and is licensed under CC BY 4.0 ↵
- “IV_Catheters_(9).JPG” by Intropin is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Simin, D., Milutinović, D., Turkulov, V., & Brkić, S. (2018). Incidence, severity and risk factors of peripheral intravenous cannula‐induced complications: An observational prospective study. Journal of Clinical Nursing, 28(9-10), 1585-1599. https://doi.org/10.1111/jocn.14760 ↵
- Gorski, L. A., Hadaway, L., Hagle, M. E., Broadhurst, D., Clare, S., Kleidon, T., Meyer, B. M., Nickel, B., Rowley, S., Sharp, E., & Alexander, M. A. (2021). Infusion therapy standards of practice. Journal of Infusion Nursing, 44(Suppl 1S), S1–S224. https://doi: 10.1097/NAN.0000000000000396.org ↵
- Gorski, L. A., Hadaway, L., Hagle, M. E., Broadhurst, D., Clare, S., Kleidon, T., Meyer, B. M., Nickel, B., Rowley, S., Sharp, E., & Alexander, M. A. (2021). Infusion therapy standards of practice. Journal of Infusion Nursing, 44(Suppl 1S), S1–S224. https://doi: 10.1097/NAN.0000000000000396.org ↵
- Gorski, L. A., Hadaway, L., Hagle, M. E., Broadhurst, D., Clare, S., Kleidon, T., Meyer, B. M., Nickel, B., Rowley, S., Sharp, E., & Alexander, M. A. (2021). Infusion therapy standards of practice. Journal of Infusion Nursing, 44(Suppl 1S), S1–S224. https://doi: 10.1097/NAN.0000000000000396.org ↵
- Gorski, L. A., Hadaway, L., Hagle, M. E., Broadhurst, D., Clare, S., Kleidon, T., Meyer, B. M., Nickel, B., Rowley, S., Sharp, E., & Alexander, M. A. (2021). Infusion therapy standards of practice. Journal of Infusion Nursing, 44(Suppl 1S), S1–S224. https://doi: 10.1097/NAN.0000000000000396.org ↵
- Wang, J., Li, M. M., Zhou, L. P., Xie, R. H., Pakhale, S., Krewski, D., & Wen, S. W. (2022). Treatment for grade 4 peripheral intravenous infiltration with type 3 skin tears: A case report and literature review. International Wound Journal, 19(1), 222–229. https://doi.org/10.1111/iwj.13624 ↵
- Gorski, L. A., Hadaway, L., Hagle, M. E., Broadhurst, D., Clare, S., Kleidon, T., Meyer, B. M., Nickel, B., Rowley, S., Sharp, E., & Alexander, M. A. (2021). Infusion therapy standards of practice. Journal of Infusion Nursing, 44(Suppl 1S), S1–S224. https://doi: 10.1097/NAN.0000000000000396.org ↵
- Gorski, L. A., Hadaway, L., Hagle, M. E., Broadhurst, D., Clare, S., Kleidon, T., Meyer, B. M., Nickel, B., Rowley, S., Sharp, E., & Alexander, M. A. (2021). Infusion therapy standards of practice. Journal of Infusion Nursing, 44(Suppl 1S), S1–S224. https://doi: 10.1097/NAN.0000000000000396.org ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
Many diseases have a genetic component. It is important to understand the risk and likelihood of a patient developing illnesses based on their family health. Ask about the health status, age, and, if applicable, cause of death of immediate blood relatives (parents, grandparents, and siblings). Questions to ask include the following:
- Tell me about the health of your blood relatives. Does anyone have diseases like cancer, heart problems, or respiratory problems?
- Have any of your blood relatives died? If so, do you know the cause of death? What age did they die?
Many diseases have a genetic component. It is important to understand the risk and likelihood of a patient developing illnesses based on their family health. Ask about the health status, age, and, if applicable, cause of death of immediate blood relatives (parents, grandparents, and siblings). Questions to ask include the following:
- Tell me about the health of your blood relatives. Does anyone have diseases like cancer, heart problems, or respiratory problems?
- Have any of your blood relatives died? If so, do you know the cause of death? What age did they die?
Occurs when a small part of the cannula breaks off and flows into the vascular system.
Functional health assessment collects data related to the patient’s functioning and their physical and mental capacity to participate in Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs). Activities of Daily Living (ADLs) are daily basic tasks that are fundamental to everyday functioning (e.g., hygiene, elimination, dressing, eating, ambulating/moving). See Figure 2.2[1] for an illustration of ADLs.
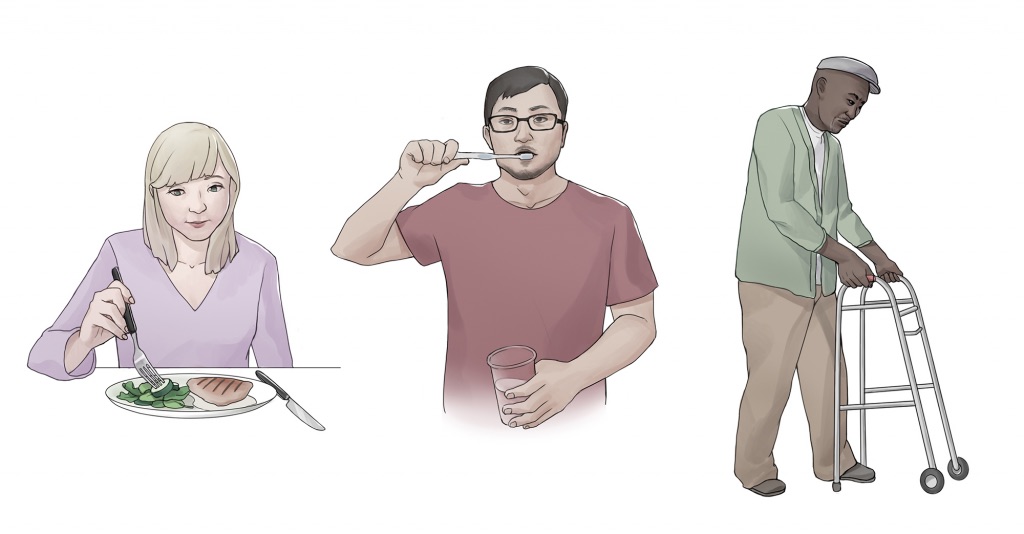
Instrumental Activities of Daily Living (IADL) are more complex daily tasks that allow patients to function independently such as managing finances, paying bills, purchasing and preparing meals, managing one’s household, taking medications, and facilitating transportation. See Figure 2.3[2] for an illustration of IADLs. Assessment of IADLs is particularly important to inquire about with young adults who have just moved into their first place, as well as with older patients with multiple medical conditions and/or disabilities.

Information obtained when assessing functional health provides the nurse a holistic view of a patient’s human response to illness and life conditions. It is helpful to use an assessment framework, such as Gordon’s Functional Health Patterns,[3] to organize interview questions according to evidence-based patterns of human responses. Using this framework provides the patient and their family members an opportunity to identify health-related concerns to the nurse that may require further in-depth assessment. It also verifies patient understanding of conditions so that misperceptions can be clarified. This framework includes the following categories:
- Nutritional-Metabolic: Food and fluid consumption relative to metabolic need
- Elimination: Excretion including bowel and bladder
- Activity-Exercise: Activity and exercise
- Sleep-Rest: Sleep and rest
- Cognitive-Perceptual: Cognition and perception
- Role-Relationship: Roles and relationships
- Sexuality-Reproductive: Sexuality and reproduction
- Coping-Stress Tolerance: Coping and effectiveness of managing stress
- Value-Belief: Values, beliefs, and goals that guide choices and decisions
- Self-Perception and Self-Concept: Self-concept and mood state[4]
- Health Perception-Health Management: A patient’s perception of their health and well-being and how it is managed. This is an umbrella category of all the categories above and underlies performing a health history.
The functional health section can be started by saying, “I would like to ask you some questions about factors that affect your ability to function in your day-to-day life. Feel free to share any health concerns that come to mind during this discussion.” Focused interview questions for each category are included in Table 2.8. Each category is further described below.
Nutrition
The nutritional category includes, but is not limited to, food and fluid intake, usual diet, financial ability to purchase food, time and knowledge to prepare meals, and appetite. This is also an opportune time to engage in health promotion discussions about healthy eating. Be aware of signs for malnutrition and obesity, especially if rapid and excessive weight loss or weight gain have occurred.
Life Span Considerations
When assessing nutritional status, the types of questions asked and the level of detail depend on the developmental age and health of the patient. Family members may also provide important information.
- Infants: Ask parents about using breast milk or formula, amount, frequency, supplements, problems, and introductions of new foods.
- Pregnant women: Include questions about the presence of nausea and vomiting and intake of folic acid, iron, omega-3 fatty acids, vitamin D, and calcium.
- Older adults or patients with disabling illnesses: Inquire about the ability to purchase and cook their food, decreased sense of taste, ability to chew or swallow foods, loss of appetite, and enough fiber and nutrients.[5]
Elimination
Elimination refers to the removal of waste products through the urine and stool. Health care professionals refer to urinating as voiding and stool elimination as having a bowel movement. Familiar terminology may need to be used with patients, such as “pee” and “poop.”
Constipation commonly occurs in hospitalized patients, so it is important to assess the date of their last bowel movement and monitor the frequency, color, and consistency of their stool.
Assess urine concentration, frequency, and odor, especially if concerned about urinary tract infection or incontinence. Findings that require further investigation include dysuria (pain or difficulty upon urination), blood in the stool, melena (black, tarry stool), constipation, diarrhea, or excessive laxative use.[6]
Life Span Considerations
When assessing elimination, the types of questions asked and the level of detail depends on the developmental age and health of the patient.
Toddlers: Ask parents or guardians about toilet training. Toilet training takes several months, occurs in several stages, and varies from child to child. It is influenced by culture and depends on physical and emotional readiness, but most children are toilet trained between 18 months and three years.
Older Adults: Constipation and incontinence are common symptoms associated with aging. Additional focused questions may be required to further assess these issues.[7]
Mobility, Activity, and Exercise
Mobility refers to a patient’s ability to move around (e.g., sit up, sit down, stand up, walk). Activity and exercise refer to informal and/or formal activity (e.g., walking, swimming, yoga, strength training). In addition to assessing the amount of exercise, it is also important to assess activity because some people may not engage in exercise but have an active lifestyle (e.g., walk to school or work in a physically demanding job).
Findings that require further investigation include insufficient aerobic exercise and identified risks for falls.[8]
Life Span Considerations
Mobility and activity depend on developmental age and a patient’s health and illness status. With infants, it is important to assess their ability to meet specific developmental milestones at each well-baby visit. Mobility can become problematic for patients who are ill or are aging and can result in self-care deficits. Thus, it is important to assess how a patient’s mobility is affecting their ability to perform ADLs and IADLs.[9]
Sleep and Rest
The sleep and rest category refers to a patient’s pattern of rest and sleep and any associated routines or sleeping medications used. Although it varies for different people and their life circumstances, obtaining eight hours of sleep every night is a general guideline. Findings that require further investigation include disruptive sleep patterns and reliance on sleeping pills or other sedative medications.[10]
Life Span Considerations
Older Adults: Disruption in sleep patterns can be especially troublesome for older adults. Assessing sleep patterns and routines will contribute to collaborative interventions for improved rest.[11]
Cognitive and Perceptual
The cognitive and perceptual category focuses on a person’s ability to collect information from the environment and use it in reasoning and other thought processes. This category includes the following:
- Adequacy of vision, hearing, taste, touch, feeling, and smell
- Any assistive devices used
- Pain level and pain management
- Cognitive functional abilities, such as orientation, memory, reasoning, judgment, and decision-making[12]
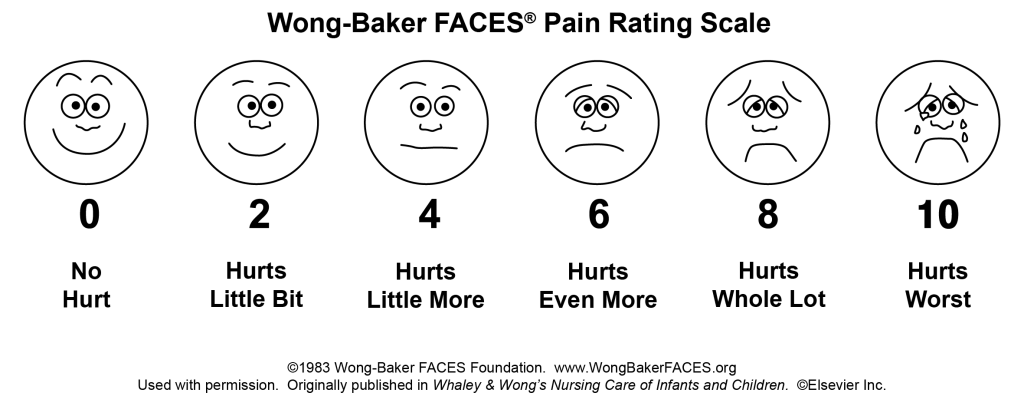
If a patient is experiencing pain, it is important to perform an in-depth assessment using the PQRSTU method described in the “Reason for Seeking Health Care” section of this chapter. It is also helpful to use evidence-based assessment tools when assessing pain, especially for patients who are unable to verbally describe the severity of their pain. See Figure 2.4[13] for an image of the Wong-Baker FACES tool that is commonly used in health care.
Life Span Considerations
Older Adults: Older adults are especially at risk for problems in the cognitive and perceptual category. Be alert for cues that suggest deficits are occurring that have not been previously diagnosed.
Roles - Relationships
Quality of life is greatly influenced by the roles and relationships established with family, friends, and the broader community. Roles often define our identity. For example, a patient may describe themselves as a “mother of an 8-year-old.” This category focuses on roles and relationships that may be influenced by health-related factors or may offer support during illness.[14] Findings that require further investigation include indications that a patient does not have any meaningful relationships or has “negative” or abusive relationships in their lives.
Life Span Considerations
Be sensitive to cues when assessing individuals with any of the following characteristics: isolation from family and friends during crisis, language barriers, loss of a significant person or pet, loss of job, significant home care needs, prolonged caregiving, history of abuse, history of substance abuse, or homelessness.[15]
Sexuality - Reproduction
Sexuality and sexual relations are an aspect of health that can be affected by illness, aging, and medication. This category includes a person’s gender identity and sexual orientation, as well as reproductive issues. It involves a combination of emotional connection, physical companionship (holding hands, hugging, kissing) and sexual activity that impact one’s feeling of health.[16]
The Joint Commission has defined terms to use when caring for diverse patients. Gender identity is a person’s basic sense of being male, female, or other gender.[17] Gender expression are characteristics in appearance, personality, and behavior that are culturally defined as masculine or feminine.[18] Sexual orientation is the preferred term used when referring to an individual’s physical and/or emotional attraction to the same and/or opposite gender.[19] LGBTQ is an acronym standing for the lesbian, gay, bisexual, transgender, and queer population. It is an umbrella term that generally refers to a group of people who are diverse in gender identity and sexual orientation. It is important to provide a safe environment to discuss health issues because the LGBTQ population experiences higher rates of smoking, alcohol use, substance abuse, HIV and other STD infections, anxiety, depression, suicidal ideation and attempts, and eating disorders as a result of stigma and marginalization.[20]
Life Span Considerations
Although sexuality is frequently portrayed in the media, individuals often consider these topics as private subjects. Use sensitivity when discussing these topics with different age groups across cultural beliefs while maintaining professional boundaries.
Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community.
Coping-Stress Tolerance
Individuals experience stress that can lead to dysfunction if not managed in a healthy manner. Throughout life, healthy and unhealthy coping strategies are learned. Coping strategies are behaviors used to manage anxiety. Effective strategies control anxiety and lead to problem-solving but ineffective strategies can lead to abuse of food, tobacco, alcohol, or drugs.[21] Nurses teach and reinforce effective coping strategies.
Substance Use and Abuse
Alcohol, tobacco products, marijuana, and drugs are often used as ineffective coping strategies. It is important to use a nonjudgmental approach when assessing a patient’s use of substances, so they do not feel stigmatized. Substance abuse can affect people of all ages. Make a distinction between use and abuse as you assess frequency of use and patterns of behavior. Substance abuse often causes disruption in everyday function (e.g., loss of employment, deterioration of relationships, or precarious living circumstances) because of dependence on a substance. Action is needed if patients indicate that they have a problem with substance use or show signs of dependence, addiction, or binge drinking.[22]
Life Span Considerations
Some individuals are at increased risk for problems with coping strategies and stress management. Be sensitive to cues when assessing individuals with characteristics such as uncertainty in medical diagnosis or prognosis, financial problems, marital problems, poor job fit, or few close friends and family members.[23]
Value-Belief
This category includes values and beliefs that guide decisions about health care and can also provide strength and comfort to individuals. It is common for a person’s spirituality and values to be influenced by religious faith. A value is an accepted principle or standard of an individual or group. A belief is something accepted as true with a sense of certainty. Spirituality is a way of living that comes from a set of values and beliefs that are important to a person. The Joint Commission asks health care professionals to respect patients’ cultural and personal values, beliefs, and preferences and accommodate patients’ rights to religious and other spiritual services.[24] When performing an assessment, use open-ended questions to allow the patient to share values and beliefs they believe are important. For example, ask, “I am interested in your spiritual and religious beliefs and how they relate to your health. Can you share with me any spiritual beliefs or religious practices that are important to you during your stay?”
Self-Perception and Self-Concept
The focus of this category is on the subjective thoughts, feelings, and attitudes of a patient about themself. Self-concept refers to all the knowledge a person has about themself that makes up who they are (i.e., their identity). Self-esteem refers to a person’s self-evaluation of these items as being worthy or unworthy. Body image is a mental picture of one’s body related to appearance and function. It is best to assess these items toward the end of the interview because you will have already collected data that contributes to an understanding of the patient’s self-concept. Factors that influence a patient’s self-concept vary from person to person and include elements of life they value, such as talents, education, accomplishments, family, friends, career, financial status, spirituality, and religion.[25] The self-perception and self-concept category also focuses on feelings and mood states such as happiness, anxiety, hope, power, anger, fear, depression, and control.[26]
Life Span Considerations
Some individuals are at risk for problems with self-perception and self-concept. Be sensitive to cues when assessing individuals with characteristics such as uncertainty regarding a medical diagnosis or surgery, significant personal loss, history of abuse or neglect, loss of body part or function, or history of substance abuse.[27]
Violence and Trauma
There are many types of violence that a person may experience, including neglect or physical, emotional, mental, sexual, or financial abuse. You are legally mandated to report suspected cases of child abuse or neglect, as well as suspected cases of elder abuse. At any time, if you or the patient is in immediate danger, follow agency policy and procedure.
Trauma results from violence or other distressing events in a life. Collaborative intervention with the patient is required when violence and trauma are identified. People respond in different ways to trauma. It is important to use a trauma-informed approach when caring for patients who have experienced trauma. For example, a patient may respond to the traumatic situation in a way that seems unfitting (such as with laughter, ambivalence, or denial). This does not mean the patient is lying but can be a symptom of trauma. To reduce the effects of trauma, it is important to implement collaborative interventions to support patients who have experienced trauma.[28]
Loss of Body Part
A person can have negative feelings or perceptions about the characteristics, function, or limits of a body part as a result of a medical condition, surgery, trauma, or mental condition. Pay attention to cues, such as neglect of a body part or negative comments about a body part and use open-ended questions to obtain additional information.
Mental Health
Mental health is frequently underscreened and unaddressed in health care. The mental health of all patients should be assessed, even if they appear well or state they have no mental health concerns so that any changes in condition are quickly noticed and treatment implemented. Mental health includes emotional and psychological symptoms that can affect a patient's day-to-day ability to function. The World Health Organization (2014) defines mental health as “a state of well-being in which every individual realizes their own potential, can cope with normal stresses of life, can work productively and fruitfully, and is able to make a contribution to their community.”[29] Mental illness includes conditions diagnosed by a health care provider, such as depression, anxiety, addiction, schizophrenia, post-traumatic stress disorder, and others. Mental illness can disrupt everyday functioning and affect a person’s employment, education, and relationships.
It is helpful to begin this component of a mental health assessment with a statement such as, “Mental health is an important part of our lives, so I ask all patients about their mental health and any concerns or questions they may have.”[30] Be attentive of critical findings that require intervention. For example, if a patient talks about feeling hopeless or depressed, it is important to screen for suicidal thinking. Begin with an open-ended question, such as, “Have you ever felt like hurting yourself?” If the patient responds with a “Yes,” then progress with specific questions that assess the immediacy and the intensity of the feelings. For example, you may say, “Tell me more about that feeling. Have you been thinking about hurting yourself today? Have you put together a plan to hurt yourself?” When assessing for suicidal thinking, be aware that a patient most at risk is someone who has a specific plan about self-harm and can specify how and when they will do it. They are particularly at risk if planning self-harm within the next 48 hours. The age of the patient is not a factor in this determination of risk. If you believe the patient is at high risk, do not leave the patient alone. Collaborate with them regarding an immediate plan for emergency care.[31]
Health Perception-Health Management
Health perception-health management is an umbrella term encompassing all of the categories described above, as well as environmental health.
Environmental Health
Environmental health refers to the safety of a patient’s physical environment, also called a social determinant of health. Examples of environmental health include, but are not limited to, exposure to violence in the home or community; air pollution; and availability of grocery stores, health care providers, and public transportation. Findings that require further investigation include a patient living in unsafe environments.[32]
See Table 2.8 for sample focused questions for all categories related to functional health.[33]
Table 2.8 Focused Interview Questions for Functional Health Categories[34]
Begin this section by saying, "I would like to ask you some questions about factors that affect your ability to function in your day-to-day life. Feel free to share any health concerns that come to mind during this discussion.”
| Category | Focused Questions |
|---|---|
| Nutrition | Tell me about your diet.
What foods do you usually eat? What fluids do you usually drink every day? What have you eaten in the last 24 hours? Is this typical of your usual eating pattern? Tell me about your appetite. Have you had any changes in your appetite? Do you have any goals related to your nutrition? Do you have any financial concerns about purchasing food? Are you able to prepare the meals you want to eat? |
| Elimination | When was your last bowel movement?
Do you have any problems with constipation, diarrhea, or incontinence? Do you take laxatives or stool softeners? Do you have any problems urinating, such as frequent urination or burning on urination? Do you ever experience leaking or dribbling of urine? |
| Mobility, Activity, and Exercise | Tell me about your ability to move around.
Do you have any problems sitting up, standing up, or walking? Do you use any mobility aids (e.g., cane, walker, wheelchair)? Tell me about the activity and/or exercise in which you engage. What type? How frequent? For how long? |
| Sleep and Rest | Tell me about your sleep routine. How many hours of sleep do you usually get?
Do you feel rested when you awaken? Do you do anything to wind down before you go to bed (e.g., watch TV, read)? Do you take any sleeping medication? Do you take any naps during the day? |
| Cognitive and Perceptual | Are you having any pain?
Note: If present, use the PQRSTU method to further assess pain. Are you having any issues with seeing, hearing, smelling, tasting, or feeling things? Have you noticed any changes in memory or problems concentrating? Have you noticed any changes in the ability to make decisions? What is the easiest way for you to learn (e.g., written materials, explanations, or learning-by-doing)? |
| Roles and Relationships | Tell me about the most influential relationships in your life with family and friends.
How do these relationships influence your day-to-day life, health, and illness? Who are the people with whom you talk to when you require support or are struggling in your life? Do you have family or others dependent on you? Have you had any recent losses of someone important to you, a pet, or a job? Do you feel safe in your current relationship? |
| Sexuality-Reproduction | The expression of love and caring in a sexual relationship and creation of family are often important aspects in a person’s life. Do you have any concerns about your sexual health?
Tell me about the ways that you ensure your safety when engaging in intimate and sexual practices. |
| Coping-Stress | Tell me about the stress in your life.
Have you experienced a recent loss in your life that has impacted you? How do you cope with stress? |
| Values-Belief | I am interested in your spiritual and religious beliefs and how they relate to your health. Can you share with me any spiritual beliefs or religious practices that are important to you? |
| Self-Perception and Self-Concept |
Tell me what makes you who you are. How would you describe yourself? Have you noticed any changes in how you view your body or the things you can do? Are these a problem for you? Have you found yourself feeling sad, angry, fearful, or anxious? What helps you to feel better when this happens? Have you ever used any tobacco products (e.g., cigarettes, pipes, vaporizers, hookah)? If so, how much? How much alcohol do you drink every week? Have you used cannabis products? If so, how often do you use them? Have you ever used drugs or prescription drugs that were not prescribed for you? If so, what type? Have you ever felt you had a problem with any of these substances because they affected your daily life? If so, tell me more. Do you want to quit any of these substances? Many patients have experienced violence or trauma in their lives. Have you experienced any violence or trauma in your life? How has it affected you? Would you like to talk with someone about it?
|
| Health Perception - Health Management |
Tell me about how you take care of yourself and manage your home. Have you had any falls in the past six months? Do you have enough finances to pay your bills and purchase food, medications, and other needed items? Do you have any current or future concerns about being able to function independently? Tell me about where you live. Do you have any concerns about safety in your home or neighborhood? Tell me about any factors in your environment that may affect your health. Do you have any concerns about how your environment is affecting your health? |

